 |
 |
AbstractPurposeTo compare photon thunderbird with deep match (technique 1) with 3-field technique with electron inguinal boost (technique 2) in acute skin toxicity, toxicity-related treatment breaks and patterns of failure in elective inguinal radiation therapy (RT) for curative chemoradiation in anal cancer.
Materials and MethodsSeventeen patients treated between January 2008 and September 2010 without evidence of inguinal and distant metastasis were retrospectively reviewed. In 9 patients with technique 1, dose to inguinal and whole pelvis area was 41.4 to 45 Gy and total dose was 59.4 Gy. In 8 patients with technique 2, doses to inguinal, whole pelvis, gross tumor were 36 to 41.4 Gy, 36 to 41.4 Gy, and 45 to 54 Gy, respectively. The median follow-up period was 27.6 and 14.8 months in group technique 1 and 2, respectively.
ResultsThe incidences of grade 3 radiation dermatitis were 56% (5 patients) and 50% (4 patients), dose ranges grade 3 dermatitis appeared were 41.4 to 50.4 Gy and 45 to 54 Gy in group technique 1 and 2, respectively (p = 0.819). The areas affected by grade 3 dermatitis in 2 groups were as follow: perianal and perineal areas in 40% and 25%, perianal and inguinal areas in 0% and 50%, and perianal area only in 60% and 25%, respectively (p = 0.196). No inguinal failure has been observed.
IntroductionFor anal cancer, nonrandomized comparisons of radical resection with radiation-chemotherapy combination, or with radiation alone, have shown that radiation-based treatment strategies produce survival rates at least equal to those of surgical series, while allowing the preservation of anorectal function in most patients [1,2]. Recent randomized trials established that the combination of radiation therapy (RT), 5-fluorouracil (5FU), and mitomycin C is the standard [2-5].
Determining the radiation volume, treatment of the primary tumor and regional lymph nodes areas is recommended for all squamous cell cancers, except superficial well-differentiated tumor less than 2 cm in size [6]. Regional lymph nodes areas are inguinal, pararectal, and internal iliac nodes. But the irregularities and the curvatures of the perineum and the lower pelvis make homogeneous radiation distributions hard to achieve.
One of the techniques to cover the primary tumor and regional lymph nodes areas is photon through-and-through. It consists of an anterior and posterior opposed field and is the simplest technique, but large volume of bowel and bilateral femur heads are fully irradiated [7]. To reduce the irradiated volume, the 'thunderbird' technique is conceived [8]. Basically, variations of thunderbird technique have the same field arrangements; an anterior field covering the pelvis and inguinal area and narrowed posterior field. An additional anterior field with partial transmission block is necessary to cover the inguinal areas, because the posterior field does not include them. Before the computed tomography (CT)-based planning era, the additional photon fields were usually matched on the anterior skin surface (photon thunderbird with skin match) [7]. The problem with this technique is the possibility of underdosage in inguinal area. By CT-based planning, the additional anterior field can be matched to the divergent edge of the posterior pelvis field at the posterior edge of the femoral vessels (photon thunderbird with deep match) [7]. To reduce irradiated bowel volume, the technique moves on to the posterior pelvis technique using 3-field technique with electron inguinal boost [9].
However, regardless of technique, grade 3 to 4 skin toxicity was common as 48% to 57% with non-intensity modulated radiotherapy (IMRT) technique and was also a common dose-limiting structure during treatment for anal cancer [3,4]. A main reason for this is skin folds in the perineal, perianal, genital, and inguinal regions and these are common sites of skin toxicity. Furthermore, patients with treatment breaks or failure to complete RT because of treatment-associated acute toxicity resulted in inferior treatment outcomes [10,11].
The purpose of the present study is to compare following 2 CT-based techniques; photon thunderbird with deep match (technique 1) and 3-field technique with electron inguinal boost (technique 2), in acute skin toxicity, toxicity-related treatment breaks and patterns of failure.
Materials and Methods1. Patients and tumor characteristicsBetween January 2008 and September 2010, 17 patients with squamous cell carcinoma of the anus without evidence of inguinal node metastasis and extra-pelvic distant metastasis were referred for curative chemoradiation. Their medical records and test results were retrospectively reviewed. The pretreatment evaluation included physical examination, routine laboratory tests, chest radiography, CT or magnetic resonance image (MRI) of abdomen-pelvis, sigmoidoscopy and tumor biopsy. In some patients, positron-emission tomography was performed. Fine needle aspiration was performed if inguinal node metastasis was clinically suspected. The tumors were staged according to the 2010 American Joint Committee on Cancer (AJCC) 7th edition [12]. The overall patient characteristics are given in Table 1. The median age was 55 (range, 46 to 75 years). There were 8 men and 9 women. The range of tumor size was 0.4 to 4 cm (mean, 2.4 cm). Three patients had clinically T4 stage due to vaginal and prostate involvement in 2 and 1, respectively. Synchronous lymph node metastases were observed in 7 patients (42%). Mesorectal node metastasis was shown in 3 patients, mesorectal and ipsilateral pelvic side wall node metastasis in 2, ipsilateral internal iliac node metastasis in 1, and mesorectal, ipsilateral pelvic side wall and external iliac node metastasis in 1 patient.
Comparisons of the patients and tumor characteristics between 2 groups are given in Table 2. Group technique 1 had more poorly differentiated tumors, more N+ stages, so more stage III patients, without statistical significance.
2. Treatment methods
Tables 1 and 2 contain brief treatment methods. Transanal mass excision was performed in 6 patients with stage I or II. CT-based treatment planning was performed for all 17 patients. All patients were treated in supine position with 2-hour bladder filling. The upper limit of the pelvic irradiation fields was situated between L5 and S1, and the lower limit was 2 to 2.5 cm below the anus. Fraction size was 1.8 Gy and treatment was performed 5 times per week.
1) RT plan and dose in group technique 1 (thunderbird technique)10 MV photon beams were used for antero-posterior and postero-anterior beams and anterior inguinal photon boost fields (Fig. 1). Inguinal lymph node areas were delineated in each patient for inguinal boost fields. Patients with N0, single N1 or N2 disease received 41.4 Gy and patients with multiple N2 disease received 45 Gy to whole pelvis and inguinal area.
Primary tumor areas were irradiated to 59.4 Gy. Gross metastatic lymph nodes were irradiated to 50.4 to 59.4 Gy, depending on the size and location of the gross lesion. For reduced fields, 6 MV posterior photon and 10 MV lateral opposing photon beams were used to cover primary tumor and metastatic lymph nodes, and for second cone down, 10 MV 5 photon beams were used to cover primary tumor area. In 4 patients with lymph node metastasis, field shrinkage was done twice. Exceptionally, in a patient with external iliac lymph node metastasis, anterior 2 ports of 6 MV photon beams were used to cover the gross metastatic node and 6 MV posterior photon and 10 MV lateral opposing photon beams were used to cover primary tumor.
2) RT plan and dose in group technique 2 (electron inguinal node boost technique)6 MV posterior photon and 10 MV lateral opposing photon beams were used for whole pelvis field. Each inguinal boost field was planned in octagonal shape [13], and electrons of 9 to 12 MeV were used depending on the depth of inguinal lymph node area (Fig. 2). In 5 of 8 patients, inguinal RT was given to 36 Gy and whole pelvis was to 45 Gy. In 2 patient with T1N0 disease showed less than 1.5 cm tumor size, 36 Gy of inguinal RT in both and 36 Gy and 41.4 Gy of whole pelvis irradiation in each were performed. In a patient with T4N0, inguinal and whole pelvis RT was to 41.4 Gy. For patients with stage I and II of tumor size less than 3 cm, 45 Gy to 50.4 Gy of total dose were given. Otherwise, 54 Gy of total dose was delivered to gross tumor area. 10 MV 5 photon beams were used to cover primary tumor areas for cone down plan.
3) ChemotherapyConcomitant chemotherapy was delivered to all 17 patients. 5FU and mitomycin regimen was given to 70% (12 patients), 5FU and cisplatin was to 24% (4 patients) and 5FU monotherapy was to 1 patient. Twenty-percent reduced dose was delivered to 3 patients over age 70. Two cycles of adjuvant chemotherapy was given to 1 patient with external iliac lymph node metastasis. There was no significant difference in chemotherapy between 2 groups (Table 2).
3. Follow-upDuring the treatment, patients were examined weekly to assess the area and grade of radiation dermatitis and other treatment-associated toxicities. Radiation dermatitis and other treatment-associated toxicities were assessed according to the Radiation Treatment Oncology Group (RTOG) common toxicity criteria [14] (Table 3).
The assessments of the tumor response were made 1 to 3 months after the completion of RT. CT or MRI of abdomenpelvis and colonoscopy were performed and biopsy was done if suspicious area still existed at post-RT 3 months.
The median follow-up period from the beginning of treatment for entire patients was 21.8 months (range, 11.1 to 43.6 months). The median follow-up period according to the RT technique was 27.6 months (range, 17.5 to 43.6 months) in the group technique 1 and 14.8 months (range, 11.1 to 27.2 months) in the group technique 2.
Results1. Acute toxicities and treatment breaksAll patients completed planned chemoradiation. In group technique 1, the incidence of grade 3 radiation dermatitis was 56% (5 patients). The range of radiation dose that grade 3 radiation dermatitis observed was 41.4 to 50.4 Gy. The affected areas were perianal and perineal area including vulvar or scrotal regions in 2 of 5 patients (40%) and perianal area only in 3 of 5 patients (60%) (Table 4). Thirty-three percent (3 patients) of group technique 1 had treatment breaks. Two patients with grade 3 radiation dermatitis needed breaks at the dose of 50.4 Gy for 6 and 10 days, respectively. The other patient needed 4 days treatment break because of thrombocytopenia less than 40,000/ВөL at the dose of 48.6 Gy.
In group technique 2, the incidence of grade 3 radiation dermatitis was 50% (4 patients). The range of radiation dose that grade 3 radiation dermatitis observed was 45 to 54 Gy. The affected areas were perianal and inguinal area in 2 of 4 patients (50%), perianal and perineal area in 1 of 4 (25%), and perianal area only in 1 of 4 patients (25%). None of the patients in group technique 2 needed treatment break (Table 4).
Comparing the 2 groups, there was no difference in the incidence of grade 3 radiation dermatitis (p = 0.819) and dose of grade 3 radiation dermatitis (p = 0.457). Comparison of the affected areas by grade 3 dermatitis was done for affected 5 patients with technique 1 and 4 patients with technique 2, and the difference was not statistically significant (p = 0.196) (Table 4).
2. Late complication and sphincter conservationOne patient experienced hematochezia at post-RT 2 years and 2 months. Colonoscopy was performed and grade 2 radiation proctitis was confirmed. Hemostasis to dilated blood vessel was done. The patient was in group technique 1 with 5FU/cisplatin chemotherapy. The dose to whole pelvis was 45 Gy and total dose was 59.4 Gy. None of the patients underwent colostomy. There was no leg edema and fibrosis of inguinal area.
3. Tumor responsesAfter initial response evaluation, 7 of 9 patients in group technique 1 and 6 of 8 patients in group technique 2 were considered in clinical complete remission. Rest of them underwent colonoscopic biopsies of suspicious lesions and all resulted as tumor free. Therefore, all patients gained clinical complete remission.
4. Patterns of failureTwo patients experienced recurrences. Local recurrence was observed in one patient 12.5 months after the treatment. The patient was initially T2N2M0 and treated by technique 1 with 4 days treatment break because of thrombocytopenia. After the diagnosis of recurrence, the patient was referred to another hospital for her preference.
The other patient experienced distant failure 14.7 months after the chemoradiation. The patient initially had stage T2N2 with external iliac lymph node metastasis. The locations of distant metastasis were lung and supraclavicular lymph nodes. He received palliative chemotherapy but died of the disease after 6 months after the diagnosis of recurrence.
No recurrence was observed in inguinal lymph node area.
Discussion and ConclusionThis study includes a series of 17 patients with squamous cell carcinoma of the anus without inguinal and extrapelvic metastasis, underwent curative chemoradiation including elective inguinal RT. Information from this study may be helpful in making decisions about techniques for inguinal RT and predicting treatment-associated toxicities.
The optimal dose of elective inguinal RT to control the disease is unclear. A couple of studies reported that after 30 Gy of elective inguinal RT in conventional fractionation, patients with clinically negative inguinal nodes at presentation are at minimal risk for inguinal failure [13]. The study of 233 clinical N0 patients received 40 Gy of elective inguinal RT resulted in 94.8% of inguinal control rate [15]. In our study, dose of inguinal RT varied from 36 to 45 Gy depending on the technique and stage. No inguinal failure has been observed, and the dose range seems to be acceptable.
In the beginning time of curative radiation for anal cancer, the incidence of perineal skin reaction was 70%, despite the low radiation dose [16]. Adding chemotherapy improved disease control rate but also increased the incidence of severe toxicities. In RTOG 87-04/EORTC 1289 study, overall rate of grade 3 or more toxicity was 62 to 78% depending on the chemotherapy regimen, and the rate of grade 3 or more radiation dermatitis was 55% from whole pelvis dose of 30.6 to 36 Gy. Above all, proportion of patients completed the protocol was only 79%, and the major radiation-induced dose-limiting toxicity was radiation dermatitis [5]. In addition, multiple studies suggested that patients with longer gap duration or overall treatment time had worse treatment outcome [17- 19]. From that, effort to reduce severe radiation dermatitis has been made by introducing new technique and assessing its usefulness compare to the 2-dimensional treatment planning. RTOG 98-11 study accepted CT-based 3- or 4-field technique for whole pelvis RT and despite the dose escalation of 36 Gy to the whole pelvis and 45 Gy to the true pelvis (below the level of sacroiliac joint), the incidence of grade 3 or more radiation dermatitis was reduced by 44% in total [20]. In our study, whole pelvis dose was 41.4 to 45 Gy by technique 1 and 36 to 45 Gy by technique 2, while the incidence of grade 3 or more radiation dermatitis was 56% and 50%, respectively. The slight higher incidence in our study might be due to the higher pelvic dose.
This study has limitations coming from its retrospective nature and small patient number. We cannot derive statistically significant results, but can find certain trends, which reflects that patients in each group received RT in homogeneous technique.
Comparing 2 different techniques, group technique 1 showed trend of earlier development of grade 3 radiation dermatitis despite the same dose range to the whole pelvis. Also the affected areas were tend to be wider including the perineal area while patients with technique 2 mainly showed separated affected areas as perianal and ingunal. But it is uncertain whether these factors are the whole reasons of treatment breaks in group technique 1 because of the higher total dose compared with the group technique 2.
In conclusion, photon thunderbird with deep match technique and 3-field technique with electron inguinal boost showed similar incidence of radiation dermatitis. However, photon thunderbird with deep match seems to increase the possibility of severe perineal dermatitis.
References1. Pocard M, Tiret E, Nugent K, Dehni N, Parc R. Results of salvage abdominoperineal resection for anal cancer after radiotherapy. Dis Colon Rectum 1998;41:1488вҖ“1493, PMID: 9860327.
2. Valentini V, Mantello G, Luzi S, Macchia G, Manfrida S, Smaniotto D. Cancer of the anal canal and local control. Rays 1998;23:586вҖ“594, PMID: 9932478.
3. Ajani JA, Winter KA, Gunderson LL, et al. Fluorouracil, mitomycin, and radiotherapy vs fluorouracil, cisplatin, and radiotherapy for carcinoma of the anal canal: a randomized controlled trial. JAMA 2008;299:1914вҖ“1921, PMID: 18430910.
4. Bartelink H, Roelofsen F, Eschwege F, et al. Concomitant radiotherapy and chemotherapy is superior to radiotherapy alone in the treatment of locally advanced anal cancer: results of a phase III randomized trial of the European Organization for Research and Treatment of Cancer Radiotherapy and Gastrointestinal Cooperative Groups. J Clin Oncol 1997;15:2040вҖ“2049, PMID: 9164216.
5. Flam M, John M, Pajak TF, et al. Role of mitomycin in combination with fluorouracil and radiotherapy, and of salvage chemoradiation in the definitive nonsurgical treatment of epidermoid carcinoma of the anal canal: results of a phase III randomized intergroup study. J Clin Oncol 1996;14:2527вҖ“2539, PMID: 8823332.
6. Chao KSC, Perez CA, Brady LW. Radiation oncology: management decisions. 2011, 3rd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.
7. Gilroy JS, Amdur RJ, Louis DA, Li JG, Mendenhall WM. Irradiating the groin nodes without breaking a leg: a comparison of techniques for groin node irradiation. Med Dosim 2004;29:258вҖ“264, PMID: 15528067.
8. Ma L, Chang W, Lau-Chin M, Tate EM, Boyer AL. Using static MLC fields to replace partial transmission cerrobend blocks in treatment planning of rectal carcinoma cases. Med Dosim 1998;23:264вҖ“266, PMID: 9863723.
9. Koh WJ, Chiu M, Stelzer KJ, et al. Femoral vessel depth and the implications for groin node radiation. Int J Radiat Oncol Biol Phys 1993;27:969вҖ“974, PMID: 8244831.
10. Roohipour R, Patil S, Goodman KA, et al. Squamous-cell carcinoma of the anal canal: predictors of treatment outcome. Dis Colon Rectum 2008;51:147вҖ“153, PMID: 18180997.
11. Constantinou EC, Daly W, Fung CY, Willett CG, Kaufman DS, DeLaney TF. Time-dose considerations in the treatment of anal cancer. Int J Radiat Oncol Biol Phys 1997;39:651вҖ“657, PMID: 9336145.
12. Edge SB. American Joint Committee on Cancer. AJCC cancer staging manual. 2010, 7th ed. New York: Springer.
13. Cox JD, Ang KK. Radiation oncology: rationale, technique, results. 2010, 9th ed. Philadelphia, PA: Mosby.
14. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341вҖ“1346, PMID: 7713792.
15. Touboul E, Schlienger M, Buffat L, et al. Epidermoid carcinoma of the anal canal: results of curative-intent radiation therapy in a series of 270 patients. Cancer 1994;73:1569вҖ“1579, PMID: 8156483.
16. Cho CC, Taylor CW 3rd, Padmanabhan A, et al. Squamous-cell carcinoma of the anal canal: management with combined chemo-radiation therapy. Dis Colon Rectum 1991;34:675вҖ“678, PMID: 1855424.
17. Deniaud-Alexandre E, Touboul E, Tiret E, et al. Results of definitive irradiation in a series of 305 epidermoid carcinomas of the anal canal. Int J Radiat Oncol Biol Phys 2003;56:1259вҖ“1273, PMID: 12873670.
18. Graf R, Wust P, Hildebrandt B, et al. Impact of overall treatment time on local control of anal cancer treated with radiochemotherapy. Oncology 2003;65:14вҖ“22, PMID: 12837978.
19. Weber DC, Kurtz JM, Allal AS. The impact of gap duration on local control in anal canal carcinoma treated by split-course radiotherapy and concomitant chemotherapy. Int J Radiat Oncol Biol Phys 2001;50:675вҖ“680, PMID: 11395235.
20. Ajani JA, Winter KA, Gunderson LL, et al. Prognostic factors derived from a prospective database dictate clinical biology of anal cancer: the intergroup trial (RTOG 98-11). Cancer 2010;116:4007вҖ“4013, PMID: 20564111.
Fig.В 1Beam's eye views (A) and isodose curve (B) of photon thunderbird with deep match (technique 1). 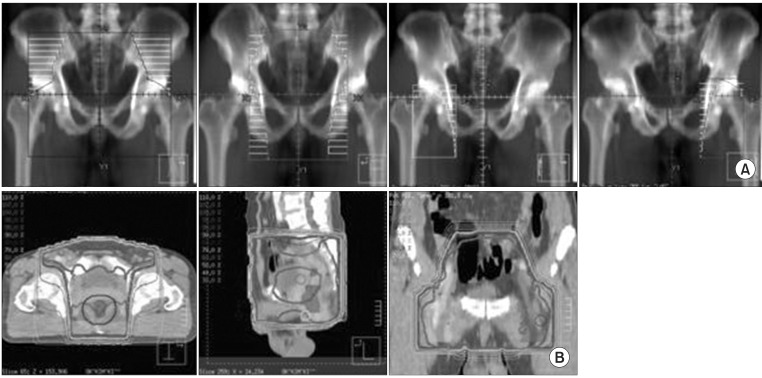
Fig.В 2Beam's eye views (A) and isodose curve (B) of 3-field technique with electron inguinal boost (technique 2). 
TableВ 3Radiation Treatment Oncology Group (RTOG) common toxicity criteria - acute skin toxicity [14] 
|
|
||||||||||||||||||||||||||||||||||||

 |
 |