 |
 |
AbstractPurposeTo investigate the coverage of axillary lymph node with tangential breast irradiation fields by using virtual lymph node (LN) analysis.
Materials and MethodsForty-eight women who were treated with whole breast irradiation after breast-conserving surgery were analyzed. The axillary and breast volumes were delineated according to the Radiation Therapy Oncology Group (RTOG) contouring atlas. To generate virtual LN contours, preoperative fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) scans with identifiable LN were fused with the CT scans, and the virtual LN contour were delineated on the CT.
ResultsThe median level I and II axillary volume coverage percentages at the VD95% line were 33.5% (range, 5.3% to 90.4%) and 0.6% (range, 0.0% to 14.6%), respectively. Thirty-one LNs in 18 patients were delineated (26 in level I and 5 in level II). In the level I axilla, 84.6% of virtual LNs were encompassed by the 95% isodose line. In the level II axilla, by contrast, none of the virtual LNs were encompassed by the 95% isodose volumes. There was a substantial discrepancy between the RTOG contouring atlas-based axillary volume analysis and the virtual LN analysis, especially for the level I axillary coverage. The axillary volume coverage was associated with the body mass index (BMI) and breast volume.
ConclusionThe tangential breast irradiation did not deliver adequate therapeutic doses to the axillary region, particularly those in the level II axilla. Patients with small breast volumes or lower BMI showed reduced axillary coverage from the tangential breast fields. For axillary LN irradiation, individualized anatomy-based radiation fields for patients would be necessary.
IntroductionStandard tangential breast irradiation technique is usually applied to patients with breast cancer after breast-conserving surgery, as it is expected to irradiate the entire breast tissue. Some investigators have reported unintentional partial irradiation of the axillary lymph node (LN) regions during tangential breast irradiation [1,2,3]. Aristei et al. [2] conducted an analysis by using surgical clips that corresponded to the level I/II axillary region. They reported that the level I and II axilla were entirely included in the tangential breast fields in 63.7%-66.7% and 45.4%-54.5% of cases, respectively. Reed et al. [1] analyzed the radiation doses delivered via tangential breast irradiation to an anatomically defined level I/II axillary region. They found that, on average, the 95% isodose line encompassed only 55% of the level I/II axillary region, and complete coverage of the level I/II axillary region by the 95% isodose line was not observed in any patient.
Because the female breast tissue lies on the anterior chest wall and is superficial to the pectoralis major muscle, the standard tangential breast fields commonly include the anterior axillary region while excluding the posterior axillary region. Despite this heterogeneous axillary coverage from the tangential breast fields, no systematic dosimetric reviews have been performed to analyze the spatial characteristics of axillary coverage. The purpose of this study was to evaluate the level I and II axillary tissue coverage by the tangential breast irradiation fields at our institution. Because a simple dosimetric axillary volume analysis could not reflect spatial information, we also investigated the virtual axillary LN coverage. Additionally, we analyzed the correlations between the patient-related factors and the axillary tissue coverage.
Materials and MethodsBetween April and June 2012, the medical records of 48 consecutive women who had been treated with tangential breast irradiation after breast-conserving surgery were analyzed. For radiotherapy (RT) planning, all patients underwent computed tomography (CT) with a 5-mm slice thickness, in a supine position with both arms overhead. The CT data were then transferred to a treatment planning system (TPS) (Eclipse 10.0; Varian Medical Systems Inc., Palo Alto, CA, USA). The clinical target volume (CTV) was defined as the entire breast tissue including the glandular breast and surrounding soft tissue. The planning target volume was defined as the CTV plus a 5-mm expansion in all directions except for the external skin surface. Treatment planning was performed with 2 tangential fields for breast irradiation. The superior margin of the fields was at the head of the clavicle. The inferior margin was at 2 cm below the inframammary fold [4]. The open tangential fields included a 1.5-2 cm flash beyond the patient's skin surface to account for the patient's breathing and setup errors. Opposing 6- or 10-MV photon beams were used for the tangential fields. The planned dose was normalized to the dose at a point 0.5-2.0 cm superficial to the chest wall-lung interface. The tangential beam wedge angles and field weights were optimized to obtain a homogenous dose distribution.
The level I and II axillary volumes and breast volumes were delineated according to the Radiation Therapy Oncology Group (RTOG) contouring atlas [5]. Axillary coverage based on RTOG contouring atlas by tangential breast irradiation were analyzed using dose-volume histograms (DVH). Axillary volumes covered by the 95% prescribed dose (VD95%) and mean dose to the level I and II axillary volume were measured. In addition, we investigated the virtual axillary LN coverage because a simple dosimetric axillary volume analysis could not reflect spatial information [6]. To acquire virtual LN contours, preoperative 18-fluorodeoxyglucose positron emission tomography/computed tomography (FDG-PET/CT) scans of patients with pathologically proven node-positive disease were evaluated.
All patients had been performed PET/CT for the purpose of clinical staging preoperatively. Preoperative PET/CT scans were acquired using a Reveal RT-HiREZ 6-slice CT scanner (CTI Molecular Imaging, Knoxville, TN, USA) or a 16-slice CT Discovery STE scanner (GE Healthcare, Milwaukee, WI, USA). Before the PET scans, for attenuation correction, a CT scans were obtained without contrast enhancement. PET scans with a maximum spatial resolution of 6.5 mm (Reveal PET/CT) or 5.5 mm (Discovery PET/CT) were obtained as well. PET images obtained using the Reveal PET/CT or Discovery PET/CT scanners were reconstructed with a 128 × 128 matrix, an ordered-subset expectation maximum iterative reconstruction algorithm (4 iterations, 8 subsets), a Gaussian filter of 5.0 mm. Slice thickness of the PET/CT was 3.0 mm (Reveal PET/CT) or 3.27 mm (Discovery PET/CT) in a supine position with both arms beside the body.
RT-planning CT and preoperative PET/CT image fusion were done using a 3D/3D auto rigid registration framework integrated into the TPS (Eclipse 10.0) based on mutual information algorithm. After auto-registration, manual adjustment was performed to compensate arm position difference between RT-planning CT (with arms overhead) and PET/CT (with arms beside the body). Specific anatomic landmarks (clavicle head, subclavian artery and vein, and the first rib) were manually matched for adjustment within two registration images, facilitating a volumetric alignment, and minimizing potential registration error.
The FDG uptake was quantified by measuring the maximum standard uptake value (SUVmax); specifically, the SUVmax was calculated as the regional radioactivity concentration divided by the injected amount of radioactivity normalized to the body weight. LNs with a SUVmax of >1.5 could be identified. By using this cutoff point, each virtual LN which was identifiable on preoperative PET/CT images was manually contoured on the RT-planning CT images by using TPS (Eclipse 10.0) (Fig. 1). PET/CT could provide a positive predictive value of >90% along with moderate sensitivity with respect to metastatic axillary LN detection [7,8]. DVHs were used to measure the 95% prescribed dose coverage (VD95%) of the virtual LNs.
The Pearson test was performed to determine the associations between the axillary coverage (VD95% of the axillary volume and the mean dose to the axillary volume) and each patient age, body mass index (BMI), breast volume, axillary volume, and lung volume. A linear regression analysis was performed to fit the axillary coverage as a function of variables above. The SPSS ver. 18.0 software package (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. Null hypotheses with no difference were rejected if the p-values were <0.05.
ResultsThe patient and tumor characteristics are presented in Table 1. Twenty-one patients underwent axillary LN dissection (ALND), and 27 patients underwent sentinel lymph node biopsy (SLNB) alone. Thirteen patients underwent immediate breast reconstruction with a myocutaneous flap. None of the patients underwent implant-based reconstruction. The prescribed whole breast irradiation dose was 50.4 Gy in 28 fractions.
The mean volumes of the level I and II axilla were 93.1 cm3 (range, 35.9 to 194.5 cm3) and 15.6 cm3 (range, 7.3 to 23.5 cm3), respectively. The mean doses to the level I and II axilla were 33.3 Gy and 14.5 Gy, respectively (Table 2). The mean coverage percentages of the level I and II axillary volumes by the 95% isodose line (VD95%) were 33.5% and 0.6%, respectively (Table 2). No patient received complete coverage of the level I and II axilla according to the 95% isodose line.
Higher BMI correlated with the increase of VD95% and mean dose to level I axilla (Fig. 2). The increase of breast volume was associated with the increase of level I axilla VD95% and mean dose to the level I and II axilla (Fig. 2). Patient age, axillary volume, and lung volume exhibited no correlation with VD95% or mean doses to the level I and II axilla.
Twenty-one of the patients had pathologically proven node-positive tumors (Table 1). Among these, 18 exhibited hypermetabolic LNs on their preoperative FDG-PET/CT scans. Thirty-one LNs from 18 patients were identified with a SUVmax of >1.5. The identified LNs images were fused with the CT images, and then they were delineated (Table 3). Among the 31 virtual LNs, 26 were located in the level I axilla and 5 in the level II axilla. In the level I axilla, 22 of 26 (84.6%) virtual LNs were encompassed by the 95% isodose volumes. In the level II axilla, by contrast, none of the virtual LNs were encompassed by the 95% isodose volumes.
Discussion and ConclusionFor many years, surgery has been a mainstay of standard axillary management for patients with invasive breast carcinoma. In the pre-sentinel node era, ALND was considered a critical component of surgery because it provided both treatment and information on nodal stage. After SLNB allowed the reliable identification of patients with axillary LN metastasis, ALND was limited to patients with axillary LN metastasis who might benefit from this procedure. For patients with sentinel LN metastasis, however, ALND has remained a standard practice.
Recently, some investigators have questioned the need for routine ALND in patients with limited sentinel LN metastasis, and they have suggested that ALND might be considered overtreatment. The prospective American College of Surgeons Oncology Group (ACOSOG) Z0011 trial [9] compared the survival rates of patients who underwent complete ALND and those treated with SLNB alone. After a median follow-up period of 6.2 years, the 5-year LN recurrence rates were 0.5% in the ALND arm and 0.9% in the SLNB alone arm (p = 0.11). No differences in the 5-year disease-free and overall survivals were observed between the groups. Recent analyses by the European Organization for the Research and Treatment of Cancer trial 10981/22023, titled 'After Mapping of the Axilla, Radiotherapy or Surgery' (AMAROS) [10], and the International Breast Cancer Study Group (IBCSG) 23-01 [11] trial were reported, and they were found to support the results of ACOSOG Z0011. The IBCSG 23-01 trial randomized patients with 1 or more micrometastatic sentinel LNs according to whether they required to undergo ALND or not. No difference in disease-free survival was observed between the group that underwent ALND and the group that did not. The AMAROS trial compared ALND and axillary RT in patients with clinically negative nodes. The researchers reported no differences in the axillary recurrence rates, overall survival, and disease-free survival between the groups. Lymphedema was observed significantly more often after ALND than after axillary RT. The interpretation of the low axillary recurrence rates in the non-ALND groups from the ACOSOG Z0011 and IBCSG 23-01 trials suggested that tangential breast irradiation and systemic therapy might contribute to the low axillary recurrence rate in patients who did not undergo ALND. To confirm this interpretation and adapt to new treatment policies of not performing ALND in patients with limited sentinel LN metastases, an understanding of the anatomic relationship between the axillary LNs and the radiation fields used in breast-conserving treatments is necessary.
In our study, a substantial discrepancy was observed between the RTOG contouring atlas-based axillary volume contour data and data from the virtual LN, particularly with respect to level I axillary coverage. In the virtual LN analysis, 84.6% of the level I axillary LNs were encompassed by the 95% isodose line, whereas the RTOG atlas-based level I axillary volume analysis revealed that, on average, only 33.5% of the volume was encompassed by the 95% isodose line. This discrepancy might reflect a drawback of conventional DVH analysis, which lacks specific clinical and spatial information [6]. Russo et al. [12] reported that underdosing primarily occurred in the posterior-superior axillary region. One possible explanation for the discrepancy between the virtual LN coverage and conventional DVH-calculated coverage might be that the LNs with high FDG uptake observed on PET scans were commonly located in the anterior level I axillary region. Therefore, when calculating the axillary region coverage according to the tangential breast irradiation fields, the DVH spatial information should also be considered.
Our results suggest that for the purpose of axillary treatment, the unintentional axillary coverage from the tangential breast irradiation fields was inappropriate, a finding that corresponded with the results of previous studies [1,2,3]. Notably, the increase of BMI and breast volume was associated with the increase of the axillary dose coverage. Fig. 3 demonstrated considerable difference of axillary coverage between the patients. While level I axillary volume of the patient in Fig. 3A covered more than 60% volume by 95% prescribed isodose line, those of the patient in Fig. 3B encompassed less than 10%. Russo et al. [12] reported that the axillary volume coverage increased with increasing tissue expander volumes in patients who underwent breast reconstruction. In our study, no patients underwent implant-based breast reconstruction, suggesting that the BMI and breast volume correlated with the axillary region dose coverage while using tangential breast irradiation. Particular attention should be given to axillary region treatment in patients with high BMI or large breast volumes
Some investigators have suggested that modified tangential breast fields could allow appropriate level I and II axillary coverage [13,14,15,16]. Takeda et al. [13,14] demonstrated the possibility of irradiating nearly all axillary LN regions by setting the dorsal edge of the irradiation field (on lateral-view simulator films) at the dorsal edge of the humeral head and by setting the cranial edge of the irradiation field at the caudal edge of the humeral head. Alco et al. [16] reported that multileaf collimator-modified high tangential fields could provide adequate axillary coverage. Some investigators have proposed 3-dimensional planning for axillary coverage, and they have demonstrated superior axillary coverage when compared with conventional tangential fields [15,17].
In summary, the virtual LN analysis revealed that tangential breast irradiation did not deliver therapeutic doses adequately to the axillary LNs, particularly those in the level II axilla. Of note, patients with small breast tissue volumes and low BMI showed lower axillary coverage from the tangential field. For axillary region irradiation, tangential breast irradiation alone was insufficient; therefore, the use of individualized RT field modifications or modern RT techniques selected according to each patient's anatomy and geometry will be necessary.
References1. Reed DR, Lindsley SK, Mann GN, et al. Axillary lymph node dose with tangential breast irradiation. Int J Radiat Oncol Biol Phys 2005;61:358–364, PMID: 15667953.
2. Aristei C, Chionne F, Marsella AR, et al. Evaluation of level I and II axillary nodes included in the standard breast tangential fields and calculation of the administered dose: results of a prospective study. Int J Radiat Oncol Biol Phys 2001;51:69–73, PMID: 11516853.
3. Reznik J, Cicchetti MG, Degaspe B, Fitzgerald TJ. Analysis of axillary coverage during tangential radiation therapy to the breast. Int J Radiat Oncol Biol Phys 2005;61:163–168, PMID: 15629607.
4. Goyal S, Buchholz TA, Haffty BG. Breast cancer: early stage. In : Halperin EC, Wazer DE, Perez CA, Brady LW, editors. Perez and Brady's principles and practice of radiation oncology. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013, p. 1044–1140, .
5. White J, Tai A, Arthur D, et al. Breast cancer atlas for radiation therapy planning: consensus definitions [Internet]. Philadelphia, PA: Radiation Therapy Oncology Group; 2015, 2015 Feb 15. Available from: http://www.rtog.org/LinkClick.aspx?fileticket=vzJFhPaBipE%3d&tabid=236.
6. Cheng CW, Das IJ. Treatment plan evaluation using dose-volume histogram (DVH) and spatial dose-volume histogram (zDVH). Int J Radiat Oncol Biol Phys 1999;43:1143–1150, PMID: 10192366.
7. Chung A, Liou D, Karlan S, et al. Preoperative FDG-PET for axillary metastases in patients with breast cancer. Arch Surg 2006;141:783–789, PMID: 16924086.
8. Ueda S, Tsuda H, Asakawa H, et al. Utility of 18F-fluoro-deoxyglucose emission tomography/computed tomography fusion imaging (18F-FDG PET/CT) in combination with ultrasonography for axillary staging in primary breast cancer. BMC Cancer 2008;8:165PMID: 18541009.
9. Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg 2010;252:426–433, PMID: 20739842.
10. Cataliotti L CM, Christiaens MR, Nieweg OE. After mapping of the axilla: radiotherapy or surgery? (EORTC protocol 10981) [Internet]. Brussels, Belgium: European Organization for Research and Treatment of Cancer; 2001, 2015 Feb 15. Available from: http://www.eortc.be/services/doc/10981-Protocol-Version5.pdf.
11. Galimberti V, Cole BF, Zurrida S, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol 2013;14:297–305, PMID: 23491275.
12. Russo JK, Armeson KE, Rhome R, Spanos M, Harper JL. Dose to level I and II axillary lymph nodes and lung by tangential field radiation in patients undergoing postmastectomy radiation with tissue expander reconstruction. Radiat Oncol 2011;6:179PMID: 22204504.
13. Takeda A, Shigematsu N, Kondo M, et al. The modified tangential irradiation technique for breast cancer: how to cover the entire axillary region. Int J Radiat Oncol Biol Phys 2000;46:815–822, PMID: 10705001.
14. Takeda A, Shigematsu N, Ikeda T, et al. Evaluation of novel modified tangential irradiation technique for breast cancer patients using dose-volume histograms. Int J Radiat Oncol Biol Phys 2004;58:1280–1288, PMID: 15001273.
15. Ohashi T, Takeda A, Shigematsu N, et al. Dose distribution analysis of axillary lymph nodes for three-dimensional conformal radiotherapy with a field-in-field technique for breast cancer. Int J Radiat Oncol Biol Phys 2009;73:80–87, PMID: 18602764.
16. Alco G, Igdem SI, Ercan T, et al. Coverage of axillary lymph nodes with high tangential fields in breast radiotherapy. Br J Radiol 2010;83:1072–1076, PMID: 21088091.
17. Smitt MC, Goffinet DR. Utility of three-dimensional planning for axillary node coverage with breast-conserving radiation therapy: early experience. Radiology 1999;210:221–226, PMID: 9885612.
Fig. 1Delineation of a virtual lymph node. (A, B) A hypermetabolic lymph node is visible on a preoperative positron emission tomography/computed tomography (PET/CT) scan (arrow). (C) A virtual lymph node (arrow) was delineated on the planning CT scan, for radiotherapy.
Fig. 2Association of axillary volume coverage with breast volume and body mass index by simple linear regression.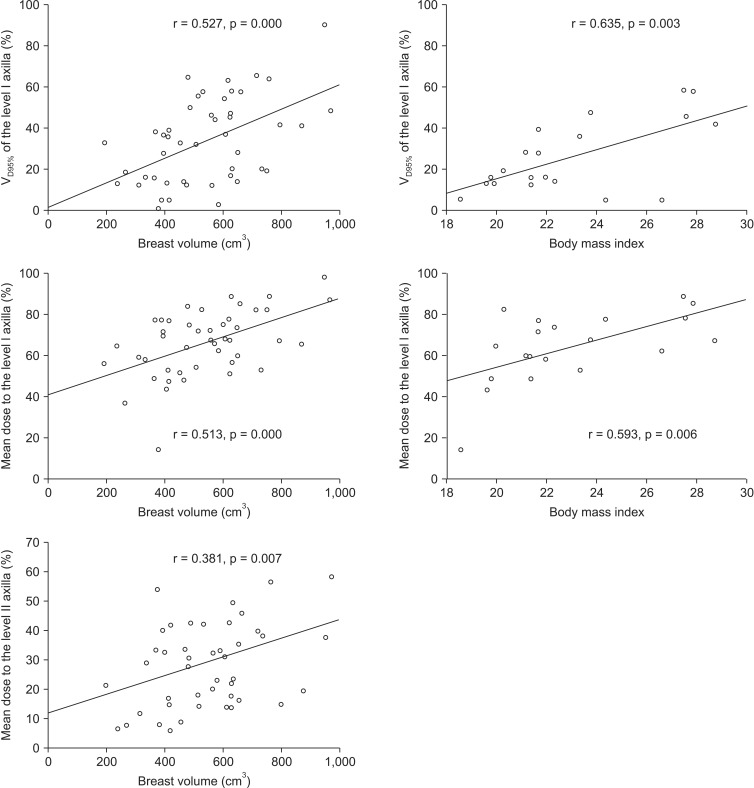
Fig. 3Axillary volume coverage by 95% prescribed isodose line in two patients. Axillary coverage was higher in the left patient (A) than in the right patient (B) by tangential breast irradiation. Blue, pink, and yellow color volumes represent level I, II, and III axilla, respectively.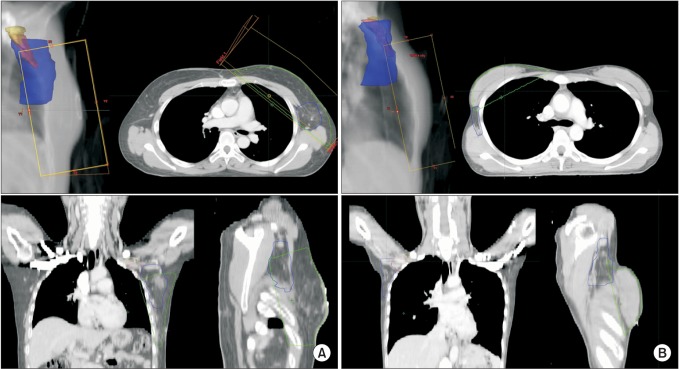
|
|
|||||||||||||||||||||||||||||||||||||||||||

 |
 |