Nationwide changes in radiation oncology travel and location of care before and during the COVID-19 pandemic
Article information
Abstract
Purpose
Patients with cancer are particularly vulnerable to coronavirus disease (COVID). Transportation barriers made travel to obtain medical care more difficult during the pandemic. Whether these factors led to changes in the distance traveled for radiotherapy and the coordinated location of radiation treatment is unknown.
Materials and Methods
We analyzed patients across 60 cancer sites in the National Cancer Database from 2018 to 2020. Demographic and clinical variables were analyzed for changes in distance traveled for radiotherapy. We designated the facilities in the 99th percentile or above in terms of the proportion of patients who traveled more than 200 miles as “destination facilities.” We defined “coordinated care” as undergoing radiotherapy at the same facility where the cancer was diagnosed.
Results
We evaluated 1,151,954 patients. There was a greater than 1% decrease in the proportion of patients treated in the Mid-Atlantic States. Mean distance traveled from place of residence to radiation treatment decreased from 28.6 to 25.9 miles, and the proportion traveling greater than 50 miles decreased from 7.7% to 7.1%. At “destination facilities,” the proportion traveling more than 200 miles decreased from 29.3% in 2018 to 24% in 2020. In comparison, at the other hospitals, the proportion traveling more than 200 miles decreased from 1.07% to 0.97%. In 2020, residing in a rural area resulted in a lower odds of having coordinated care (multivariable odds ratio = 0.89; 95% confidence interval, 0.83–0.95).
Conclusion
The first year of the COVID pandemic measurably impacted the location of U.S. radiation therapy treatment.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic had an unprecedented impact on all aspects of medical care. For cancer patients, the medical impact of the pandemic extended beyond direct infection by covid. Patients with cancer are particularly vulnerable to COVID and experience the dual impact of cancer and its treatment as well as an increased risk of infection [1]. As a result of this risk, the early response from many radiation oncology facilities was to reduce or delay radiation treatment visits [2]. Furthermore, transportation barriers made travel to obtain medical care more difficult during the pandemic [3]. Given the repeated nature of most radiation treatments, travel and transportation issues are particularly relevant for patients undergoing radiotherapy [4]. Whether these factors led to changes in where radiation oncology treatment occurred, and the distance traveled by patients for radiotherapy is unknown.
The location of radiation oncology care may also reflect overall cancer care coordination, since cancer patients can be diagnosed at one healthcare facility and treated at another. For example, patients can often present to a relatively distant academic tertiary center for workup and diagnosis but can be treated at a radiation facility closer to home. Alternatively, patients can be diagnosed at their community hospital but elect to travel further to a higher volume radiation facility for treatment. Since half of all cancer patients undergo radiation therapy at some point in their cancer care, coordination of radiation oncology care is a critical issue for study [5]. This is particularly important for patients living in rural environments, as multiple locations of care and distance traveled may be exacerbated given the geographic maldistribution of radiation oncology practice in these areas [6]. Whether the COVID-19 pandemic has impacted the coordinated location of radiation therapy receipt is unknown.
The aims of this study are therefore twofold. First, we aim to evaluate the distance traveled by patients undergoing radiotherapy in 2020 (which we define as having happened during the COVID-19 pandemic) versus 2018 and 2019. Second, we aim to evaluate whether there were changes in the proportion of patients who underwent radiation at the same facility that diagnosed their cancer in 2020 versus 2018 and 2019. For the purposes of our study, if patients underwent radiation at the same facility that diagnosed their cancer, we will consider this “coordinated care.”
Materials and Methods
1. Description of the data
The National Cancer Database (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society, that collects hospital registry data from over 1,500 accredited facilities. The database accounts for approximately 72% of U.S. cancer patients [7]. The NCDB participant user file (PUF) contains de-identified patient-level data from CoC accredited programs. For this study, disease sites were obtained for analysis encompassing the 60 most common primary disease sites for radiotherapy (Supplementary Table S1). The data includes patients diagnosed through 2020.
2. Sample construction
We analyzed only patients from 2018–2020 to evaluate the most immediate pre and during-pandemic years available. Sixty cancer sites were included (Supplementary Table S1). We excluded patients who did not have radiation treatment as recorded in RAD_LOCATION_OF_RX variable. This resulted in 1,151,954 patients (Fig. 1).
3. Construction of variables
Ten independent variables of interest were selected a priori to evaluate for association with the dependent variables: age of patients, race (White, Black, non-White other), sex, residence in a metropolitan area, residence in an area with highest quartile of median income, type of insurance, status of insurance, type of treating facility, number of Charlson Comorbidities, and stage of cancer.
Metropolitan areas were defined as counties with populations of more than 250,000 people. The highest income quartile was defined in the NCDB using the 2016 American Community Survey (ACS) data spanning 2012–2016 and indicated an area median household income of ≥$63,333.
First, for patients who received radiation at the diagnosing facility, CROWFLY, the “great circle” distance in miles between the patient's residence and the hospital that reported the case, was used as a surrogate for travel distance. Of note, distance from place of residence to radiation treatment facility was not able to be measured if a different facility from the facility that reported the cancer to the NCDB. Patients who received radiotherapy at a facility different from the diagnosing facility were excluded from the analysis of travel distance to radiotherapy centers.
Second, radiation care was designated as “coordinated” if all radiation treatment including initial and boost therapy was delivered at the diagnosing facility. All other radiation was otherwise considered not “coordinated.” RAD_LOCATION_OF_RX, which identifies the location where radiation therapy was administered during the first course of treatment, was therefore used as a surrogate for coordinated care (Supplementary Table S2). Specifically, if RAD_LOCATION_OF_RX indicated all radiation treatment occurred at the reporting facility, we designated this “coordinated care.” Care that took place in multiple locations, or radiation therapy that happened at a facility that was not the reporting facility, was not considered coordinated.
4. Statistical analysis
1) Travel distance
Descriptive statistics were performed. Travel distance was dichotomized to distant versus close travel by whether the great circle distance between the patient’s residence and radiotherapy facility was greater than 50 miles [8]. Univariate and multivariate logistic regression was performed to assess independent variables associated with distant travel. Variables were assessed for correlation using a pairwise Pearson correlation matrix. Only age and insurance status approached a strong (r = 0.48) correlation. Given lack of significant correlation, all variables were included in the multivariable analysis. Weak correlation was seen between living in a metropolitan area and an area of high average income (r = -0.28). All other correlation coefficients were <0.20.
To evaluate the association between year of diagnosis and travel on the facilities with the highest volume of patients coming from far distances, we first counted the number of patients who got treated with radiation at the same facility that reported the cancer, who traveled more than 200 miles for treatment. We designated the facilities in the 99th percentile or above in terms of the proportion of patients who traveled more than 200 miles as “destination facilities.” We measured the decrease in the proportion of patients who traveled more than 200 miles in 2020 versus 2019 in these “destination facilities” versus all other facilities.
2) Coordinated care
Coordinated care broadly means coordinated information sharing and care management between healthcare providers in diagnosis and treatment [9]. Coordinated care has been shown to improve patient survival, reduce readmission, and patient satisfaction [10-12]. Furthermore, coordinated cancer care has been investigated in the NCDB in the same manner as our study for colorectal and pancreatic cancer, showing improved overall survival [13,14]. We assume that care given by a radiation oncology facility that is also the same facility that diagnosed the cancer will have “coordinated care” through coordinated information sharing and patient management.
Descriptive statistics were performed. Univariate and stepwise multivariate logistic regression was performed to assess independent variables associated with coordinated care. To compare year over year changes, we compared the mean travel distance in 2020 compared to 2019, and in 2019 to 2018 using a t-test. We also compared the percent of patients who traveled more than 50 miles in 2020 compared to 2019, and in 2019 compared to 2018 using the chi-squared test of proportions. This was performed for all patients (and thus was analyzing patient travel to their facility of diagnosis) as well as only those who underwent radiation at the same facility that diagnosed their cancer (and so measured distance to radiation facility in these patients). We did not perform a formal trend test as we only had three time points (2018, 2019, and 2020). Given the large number of patients, we used p < 0.001 as the threshold for statistical significance.
Due to the number of disease sites involved, a subset of lung, breast, and prostate cancer was evaluated as the most common solid tumors. Cervical cancer was also evaluated as an example of particularly complex radiotherapy care as treatment often requires coordinated external beam treatment and brachytherapy. Due to the number of primary tumors evaluated (encompassing 319 unique ICD-O-3 primary tumor codes), we did not evaluate the impact of different primary tumor types on travel distance or coordinated care. Specific evaluation of selected primary tumor types is the focus of future work.
All statistical analysis was performed with STATA 17.0 (StataCorp., College Station, TX, USA). Given the large size of the evaluated dataset, statistical significance was a priori defined as p < 0.001.
Results
We evaluated 1,151,954 patients who underwent radiotherapy from 2018–2020. The absolute number of patients in our analysis declined from 2019 to 2020, from 407,525 patients in 2019 to 345,068 in 2020. This was a significant deficit and other investigators have noted this large decline as well [15].
Characteristics of patients undergoing radiation therapy were generally similar throughout 2018–2020 (Table 1). Characteristics that changed more than 1% from 2018–2019 to 2020 included a decrease in the proportion of patients treated in the Mid-Atlantic (NJ, NY, PA), decrease in the proportion of patients with private insurance or managed care, decrease in the proportion of patients treated at an academic or comprehensive cancer center, with an increase in the proportion treated at a community cancer center.
Mean distance traveled from place of residence to the facility that reported the cancer to the NCDB decreased from 30.4 miles to 28 miles in 2018 to 2020 (Table 2). The proportion traveling greater than 50 miles decreased from 9.1% to 8.6%. Mean distance traveled from place of residence to radiation treatment (if it was the same facility that reported the cancer) decreased from 28.6 to 25.9 miles, and the proportion traveling greater than 50 miles decreased from 7.7% to 7.1% (Table 3).

Distance traveled between place of residence and radiation center (if the same as reporting hospital)
Given the large size of the database, all variables were significantly associated with odds of travel more than 50 miles in 2020 in univariable logistic regression. In our multivariable logistic regression model, age, sex, metropolitan versus urban versus rural residence, Race, geographic area, income, and type of diagnosing facility were all associated significantly with travel more than 50 miles (Table 4). Patient-specific variables such as stage and comorbidity were less associated with travel more than 50 miles.

In patients who underwent radiation at the diagnosing facility, univariate and multivariate logistic regression for variables associated with >50 miles traveled, in the year 2020
Destination hospitals were those in the top 1% of proportion of patients traveling more than 200 miles. At those hospitals, the proportion traveling more than 200 miles decreased from 29.3% and 28% in 2018 and 2019 to 24% in 2020. In comparison, at the other hospitals, the proportion traveling more than 200 miles decreased from 1.07% and 1.13% to 0.97%.
Regarding coordinated radiation treatment in 2020, all variables were again associated with coordinated treatment on univariate logistic regression. In our multivariate logistic regression model, independent variables associated with geography and facility type were associated with coordinated care. Individual characteristics such as race, comorbidity, and cancer stage were less obviously associated (Table 5). While residing in a rural area had a much higher odds of traveling more than 50 miles (multivariable odds ratio [OR] = 20.9; 95% confidence interval [CI], 19.2–22.8), it also had a lower odds of having coordinated care (multivariable OR = 0.89; 95% CI, 0.83–0.95). In contrast, though patients who were treated at academic research programs including the National Cancer Institute (NCI) designated cancer centers had a much higher odds of traveling more than 50 miles (multivariable OR = 22.6; 95% CI, 20.3–25.3), they also had higher odds of coordinated care (multivariable OR = 1.53; 95% CI, 1.48–1.59). Being identified as Black was associated with a lower odds of travel (multivariable OR = 0.45; 95% CI, 0.42–0.48), and higher odds of coordinated care (multivariable OR = 1.31; 95% CI, 0.27–1.35).
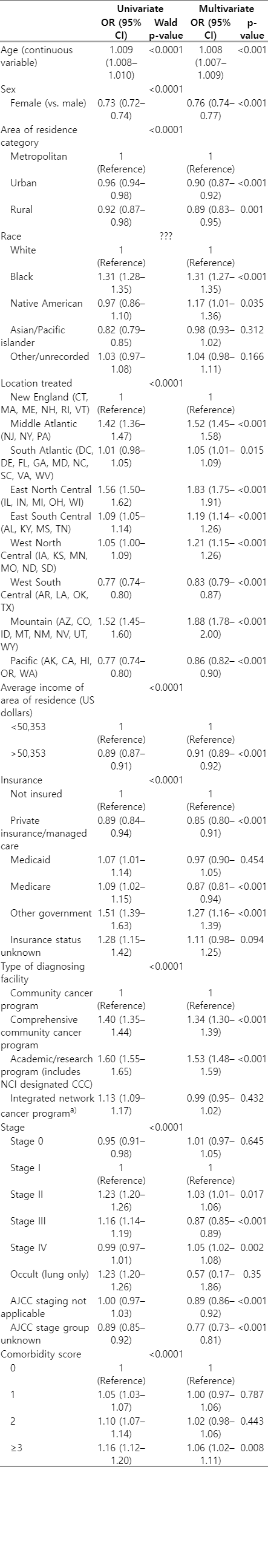
Univariate and multivariate logistic regression for variables associated with coordinated care, in the year 2020
We also performed univariate and multivariate logistic regression for patients diagnosed in 2018–2019 (Supplementary Table S3). These factors were broadly similar to patients diagnosed in 2020 with the exception that patients with Medicaid were no longer significantly less likely than those who were uninsured to have coordinated care. As well, in 2018–2019, integrated network cancer programs were not less likely to undergo coordinated care compared to the reference of the community cancer program, whereas in 2020 they were less likely to undergo coordinated care.
In regards to travel, for patients diagnosed in 2018–2019, the Mid-Atlantic States were more likely to have greater travel distance compared to New England, whereas in 2020 that difference was not statistically significant (Supplementary Table S4). Again, Medicaid patients in 2020 were equally likely to travel as those who were uninsured, whereas in 2018–2019 they were more likely to travel >50 miles for care.
Patients were statistically significantly less likely to travel more than 50 miles in 2019 compared to 2020. Furthermore, the mean travel distance was statistically significantly lower in 2020 compared to 2019. This was true for all patients in relation to their diagnosing facilities, as well as patients in relation to their radiation treatment facility (if it was the same as their diagnosing facility). There were no statistically significant differences between 2018 and 2019.
Finally, the percent of patients with lung, breast, and prostate cancer traveling more than 50 miles are reported in Table 6. Generally, patients with breast, prostate and lung cancer were less likely to travel more than 50 miles for treatment compared to all cancers (6.7%, 8.8%, and 9.1%, respectively, vs. 10.1% in 2020). Lung and prostate cancer patients were more likely to receive coordinated care in all years, whereas breast cancer patients were less likely (80.3%, 83.8%, and 70.4%, respectively, vs. 74.8% for all cancers in 2020). Cervical cancer patients were both more likely to travel more than 50 miles (13.8% in 2020 and 15.9% in 2018–2019), and also less likely to have coordinated care (69.2% in 2020 and 68.3% in 2018–2019).
Discussion and Conclusion
Though the proportions of patients traveling large distances and receiving coordinated radiation decreased only slightly from 2018 through 2020, the Mid-Atlantic States and academic centers had the greatest proportional decrease in patients radiated overall. Demographic, geographic, and facility level variables such as age, race, population density, and type of center were associated with greater travel, whereas clinical characteristics such as stage and comorbid illness were less associated. Centers who had a high proportion of patients traveling long distances for treatment experienced the greatest proportional decrease in those same patients in 2020 compared to 2018 and 2019. However, for the vast majority of radiation treatment centers, there was a minimal relative decline in the proportion of patients traveling long distances for diagnosis or radiation treatment.
These findings indicate that “destination” radiation oncology centers and academic centers experienced the greatest decrease in patient volume during the pandemic, and these patients were likely instead treated at radiation centers closer to a patient’s place of residence. Besides the expected financial implications corresponding to fluctuations in patient load, these changes may impact individual clinical care, as well. Multiple studies have shown that treatment at an academic center is associated with improved survival in a variety of types of cancer [16-20]. Moreover, a number of analyses have also demonstrated a survival benefit from being treated at a high-volume center [21-23]. Logically, higher volume may improve skill and proficiency among providers, leading to improved care. It follows that declines in the number of patients treated could eventually erode the clinical advantages at academic and destination centers, which are often high-volume facilities. While the relatively small changes we have detected are unlikely to cause significant changes in the short-term, these trends and their impact should continue to be closely monitored over time.
The changes in distance traveled may reflect the broader economic impact of the COVID-19 pandemic. For example, during the pandemic the poverty rate rose from 10.5% to 13.6% from 2019 to 2020 despite federal aid programs, resulting in an estimated 9.8 million people descending into poverty [24]. There was a reduction in available childcare, with over 70% of childcare arrangements canceled or reduced by August 2020, had disproportionate impact on low-income families [24]. At the same time, COVID-19 disrupted general access to health care with particular impact on low-income Black and Hispanic households, leading to delay of non-emergent care [25]. Preventative healthcare including cancer screenings experienced a sharp decrease in the early months of the pandemic, with incomplete rebound [26]. Given the unprecedented impact of the pandemic on national economic well-being and healthcare access, it is not surprising that our analysis reflected a decline in travel for radiation treatment.
Importantly, we found that distance traveled was associated with many socio-economic factors and less associated with disease specific factors. This is consistent with work showings socio-economic factors influence travel access to cancer care [27]. Furthermore, it is possible that we underestimated the impact of socio-economic factors on travel distance, as those with the most severe socio-economic barriers may not have received radiation at all.
We found that the common cancers of breast, prostate, and lung primary site were less likely to travel more than 50 miles than all cancers together. We hypothesize that more rare cancers or those cancers with more complex management could potentially move patients to travel longer distances whereas these relatively common cancers were readily treated at closer cancer centers. We also found that while lung and prostate cancer patients were more likely to receive coordinated care in all years, breast cancer patients were less likely (compared to all cancers) to receive coordinated care. This finding is in contradiction to conventional wisdom that reduced travel results in more coordinated care. However, it is also possible that physicians at diagnosing centers may attempt to alleviate patient travel burden by referring patients to providers closer to home, which may both reduce travel burden but also reduce coordination of care [28]. Why this would be unique to breast cancer (vs. lung and prostate cancer) is unclear, and should be the focus of future research.
Cervical cancer patients were both more likely to travel more than 50 miles as well as less likely to have coordinated care. It is possible that cervical cancer represents a more complex radiation treatment that is performed at specialized centers. One potential insight from these findings is that all radiation facilities are not created equal, and there are probably some enters that more readily treat breast, prostate, and lung cancers compared to cervical cancers. Why these differences exist between different cancer types remains unclear and should be the focus of future research.
There are several limitations to this study and its utilization of retrospective data to describe relative changes in travel for radiation treatment after the COVID-19 pandemic. The NCDB, while a large population-based database, includes only 72% of the U.S. patients with cancer which may represent a selection bias towards patients underrepresenting patients not presenting to CoC participating cancer centers. This has been previously shown to limit the generalizability of analyses when using information from this database [29]. In addition to this potential selection bias of the database itself, we excluded patients with missing data, an issue that may be exacerbated by lack of complete records during the COVID-19 pandemic. Missing data has been previously shown to indicate unfavorable outcomes [30]. In an effort to evaluate the change in practice patterns for patients receiving radiotherapy, we also excluded patients for whom radiotherapy was omitted regardless of reason. Therefore, patients who may have benefited from radiotherapy but were unable to travel at all for radiation for financial or health reasons were not included. Furthermore, we utilized diagnosis and treatment at one facility as a surrogate marker for coordinated care. Although this is a useful definition for analysis of NCDB data that implies coordination of care, true coordination of care in clinical practice is much more complex and primarily defined by effective communication between the multidisciplinary team. Thus, diagnosis and treatment at the same facility may provide a limited representation of coordinated care and influence the results reported in this analysis. Finally, 50 miles was defined as the differentiating distance for close versus far travel based upon referral patterns at our institution and may not be generalizable to different geographic areas of the country. Regardless of these limitations, our analysis supports further investigation into the vast impact of COVID on cancer care that will continue to be realized in the coming decades. A limitation of this study is the lack of knowledge regarding travel distance for patients who underwent radiation treatment at facilities that were different from the diagnosing hospitals. This data was not recorded in the NCDB. This lack of knowledge could result in a lack of reflection of actual radiation oncology travel and location for these patients. Due to the number of primary tumors evaluated (encompassing 319 unique ICD-O-3 primary tumor codes), we did not evaluate the impact of different primary tumor types on travel distance or coordinated care. Specific evaluation of selected primary tumor types is the focus of future work.
Strengths of this study include the large size of our sample, including over a million of patients and wide variety of cancer sites included. This allows for a nationwide assessment of how the pandemic impacted huge numbers of patients and facilities. Continued longitudinal studies are necessary to evaluate how travel and coordinated care changed as the COVID-19 pandemic evolved in the United States.
In conclusion, the proportion of patients treated in Middle Atlantic States with private insurance, at comprehensive cancer centers, decreased in the first year of the COVID-19 pandemic. Travel distance also declined, especially at facilities that had high levels of distant travelers in the pre-pandemic period. Further work should focus on the continued impact of the pandemic in subsequent years, and the impact of the pandemic on multidisciplinary coordination of care.
Notes
Statement of Ethics
This study used publicly available data and was exempt from institutional review.
Conflict of Interest
There are no conflicts of interest related to this work. Outside of this work, Dr. Yu reports research funding, speaking and consulting fees from Pfizer/Myovant, consulting fees from Boston Scientific, and Speaking fees from RefleXion Medical.
Funding
None.
Author Contributions
Conceptualization, Investigation and methodology, and writing of the original draft: De Leo AN, Giap F, Culbert MM, Drescher N, Brisson RJ, Cassidy V, Augistin EM, Casper A, Yu JB. Formal analysis: Yu JB. Writing of the review and editing: De Leo AN, Giap F, Culbert MM, Drescher N, Brisson RJ, Cassidy V, Augistin EM, Casper A, Horowitz DH, Cheng SK, Yu JB.
Data Availability Statement
NCDB data is publicly available for US Commission on Cancer (CoC) affiliated institutions.
Supplementary Materials
Supplementary materials can be found via https://doi.org/10.3857/roj.2023.00164.
Sixty most common primary disease sites for radiotherapy
Coordination of care code
In patients who underwent radiation at the diagnosing facility, Univariate and multivariate logistic regression for variables associated with >50 miles traveled, in the year 2018–2019
Univariate and multivariate logistic regression for variables associated with coordinated care, in the year 2018–2019




