The using of megavoltage computed tomography in image-guided brachytherapy for cervical cancer: a case report
Article information
Abstract
We present a case of cervical cancer treated by concurrent chemoradiation. In radiation therapy part, the combination of the whole pelvic helical tomotherapy plus image-guided brachytherapy with megavoltage computed tomography of helical tomotherapy was performed. We propose this therapeutic approach could be considered in a curative setting in some problematic situation as our institution.
Introduction
After the first concept of helical tomotherapy started in the late 1980s, the first patient was treated by helical tomotherapy in 2002 at the University of Wisconsin. Tomotherapy provides us the accuracy of treatment by megavoltage computed tomography (MVCT) that inter-fractionation motion can be evaluated before each fraction. After that, there were many implementations of tomotherapy in various sites of cancer [1]. In our department, helical tomotherapy (HT) was equipped during March 2012. Until now, patients with nasopharyngeal cancer, prostate cancer, cervical cancer, and others had been treated by this machine. HT was used for external beam radiation therapy (EBRT). Unfortunately, our computed tomography (CT) simulator has permanently broken without spare part since September 2014 and we are waiting for a replacement. This article reported the use of MVCT in HT for image-guided brachytherapy (IGBT) in cervical cancer.
Case Report
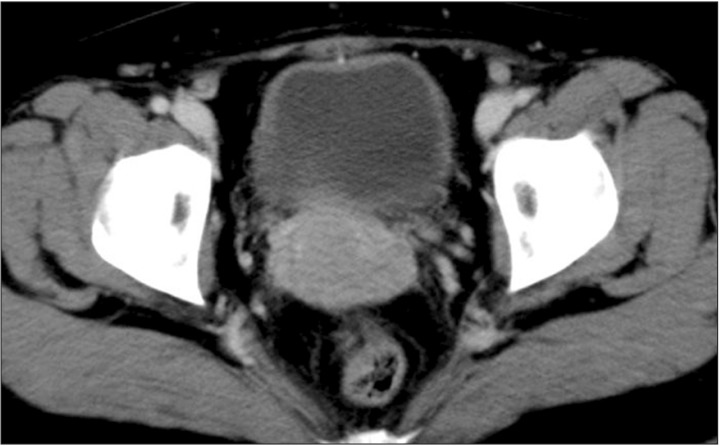
A 39-year-old woman came with abnormal vaginal discharge for 3 months. Per vaginal examination revealed 5 cm in diameter lesion on the cervix with bilateral parametrial involvement. Biopsy revealed squamous cell carcinoma, moderately differentiated. CT at pelvis reported enlarged uterine cervix with circumferential thickening of the upper vagina (Fig. 1). With discussions, she preferred to treat with HT plus IGBT. However, our CT simulator has broken since September 2014 and needed to replace with another one.
1. Whole pelvic helical tomotherapy
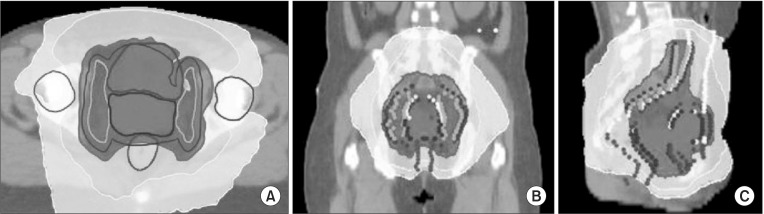
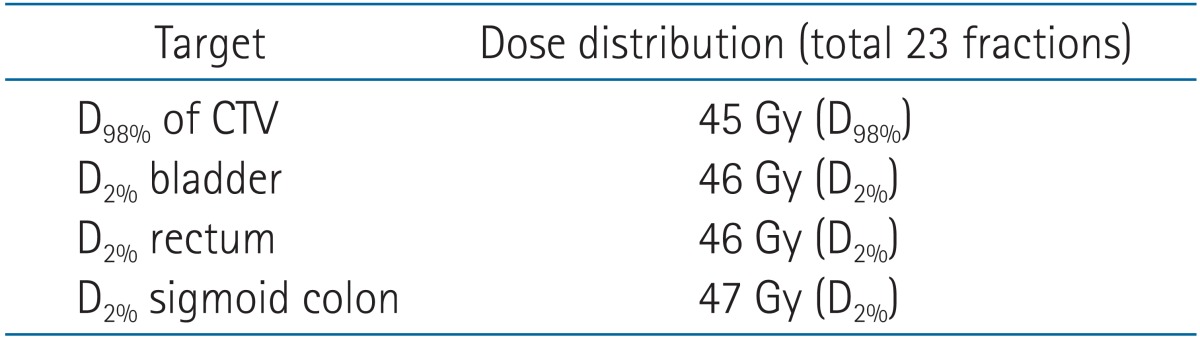
For whole pelvic helical tomotherapy (WPHT), the simulation by CT was performed at the outsource department with 5-mm slice thickness. Clinical target volume (CTV) composed of gross tumor volume, cervix, uterus, parametrium, adnexae, and elective pelvic lymph nodes (common iliac, external iliac, internal iliac and presacral lymph nodes) were contoured as the Radiation Therapy Oncology Group (RTOG) guidelines. The normal tissues (organs at risk [OARs]; bladder, rectum, sigmoid, bowels, and head of femurs) were also contoured. WPHT was done to the dose of 46 Gy in 23 fractions according to ICRU Report 83 (Fig. 2). The dose at 98% of reference volume (D98%) of CTV, D2% of the bladder, D2% of rectum, and D2% of sigmoid colon were recorded [2]. Weekly cisplatin (40 mg/m2) was prescribed to the patient with the total of five cycles. The MVCT was performed everyday to check the position before irradiation.
2. Image-guided brachytherapy
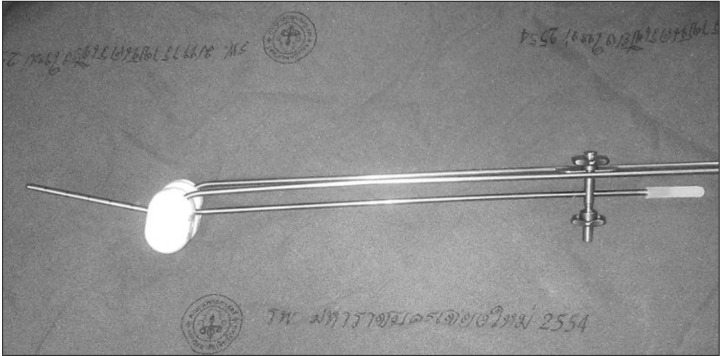
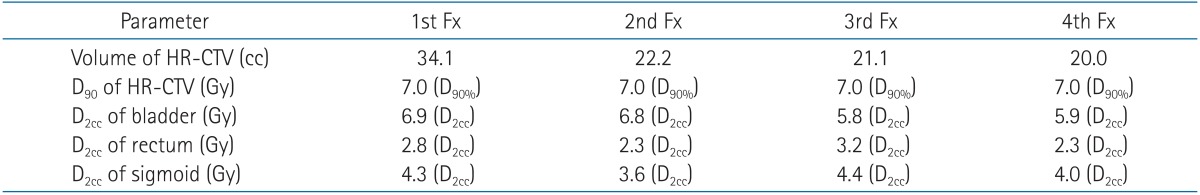
For WPHT, we can use outsource CT from our faculty branch, but it is impossible to transfer patient with applicator to that place. To solve this problem, we thought about using of the MVCT of HT situated close to our brachytherapy suite. The first brachytherapy was performed after the fourth week of EBRT. To reduce the artifact, Rotterdam Titanium applicator (Nucletron-Elekta, Stockholm, Sweden) was used (Fig. 3). A Foley catheter was placed in the bladder and filled with contrast media and normal saline solution to identify the bladder volume for imaging planning. The vagina was packed with gauze to increase the distance between the radiation source, and the rectum and bladder. The WPHT was interrupted for each day of high-dose rate (HDR) brachytherapy insertion. After application, the patient was transferred to imaging devices, and the pelvic region from the iliac crest to the ischial tuberosity was scanned without intravenous contrast to obtain appropriate images with the patients in a supine treatment position with their legs relaxed on the table. The MVCT was performed with 4-mm slice thickness without an interslice gap. After the imaging was performed the position of the applicators was checked before being transferred to the planning system (Nucletron Oncentra). Patients were then transferred to the brachytherapy treatment room and adjusted to the same position as in the imaging devices. MVCT image was used and GEC-ESTRO definitions were applied to identify target volumes, e.g., high-risk clinical target volume (HR-CTV), and OARs [345]. Dose-volume histograms were calculated to consider the adequate dose to HR-CTV and limitations of OARs. The minimum dose covering 90% of volumes (D90) of the HR-CTV and representing the maximum doses calculated at the most irradiated 2 cc volumes (D2cc) of OARs were recorded according to GEC-ESTRO recommendations. The prescribed dose to the D90 of HR-CTV was at least 7 Gy × 4 fractions. Optimizations were performed to improve the dose distribution to HR-CTV, bladder, rectum, and sigmoid colon (Fig. 4). The D90 of HR-CTV and D2cc of OARs were recorded to evaluate the cumulative dose in EQD2 concepts [6].
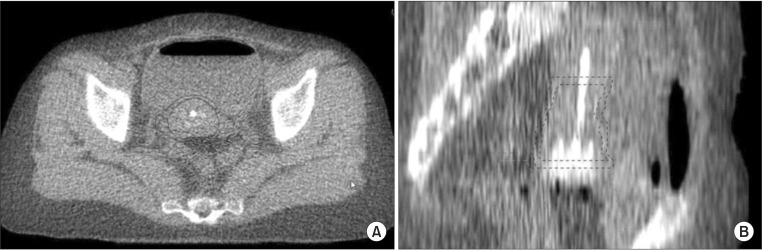
Megavoltage computed tomography image in (A) transverse and (B) sagittal views showed the contours of HR-CTV (red), IR-CTV (blue), bladder (light blue), and sigmoid colon (green). HR-CTV, high-risk clinical target volume; IR-CTV, intermediate-risk clinical target volume.
The physical doses of WPHT (CTV, bladder, rectum, and sigmoid colon) and all fractions of MVCT-based brachytherapy were reported in Tables 1 and 2.
The cumulative dose in EQD2 concept to D90 of HR-CTV, D2cc of the bladder, D2cc of the rectum, and D2cc of sigmoid colon were 84.5, 93.7, 58.1 and 70.6 Gy, respectively. During treatment, patient had no serious complication. After two months, per vaginal examination was performed and no residual tumor was seen and the patient did not complain about toxicity.
Discussion
The using of MVCT for intracavitary brachytherapy in the literatures appeared in case reports with the attempt to lessen the streak artifacts of metallic applicator that naturally occurred in kilovoltage computed tomography (kVCT).
Holly et al. [7] reported the use of MVCT imaging to plan a HDR prostate brachytherapy treatment for a patient with bilateral prostheses. They reported a 77-year-old man presented with a stage T3a, Gleason 7 prostate cancer. The pelvic CT exhibited significant streak artifacts obscuring the prostate. HDR monotherapy with adjuvant androgen deprivation therapy was proposed. On the day of the implant and after catheter insertion, MVCT imaging of the pelvic area of the patient was obtained using a commercial HT unit. The MVCT images were transferred to Nucletron PLATO (v14.3.2) for planning with optimization of catheter dwell positions and times. This study showed MVCT images allowed good visualization of bony anatomy and of the hip prosthesis. No reconstruction streak artifacts are visible in the images as seen in the diagnostic kVCT images [7].
Libby et al. [8] reported the using MVCT for a lateral oral tongue cancer. A patient was treated with HDR brachytherapy using an oral applicator with embedded lead shielding making conventional simulation, using either kVCT or radiographs, impossible because of scatter artifact. Treatment simulation was accomplished using MVCT simulation on a HT unit. VelocityAI image registration software (Velocity Medical Solutions, Atlanta, GA, USA) was used to register an MVCT of the applicator itself with the patient MVCT simulation. The treatment plan was manually optimized to prescribe 4 Gy/fraction to the gross tumor volume. The patient tolerated the treatment well, with no evidence of disease 6 months after treatment. This report showed the use of MVCT for with image registration allowed treatment planning in the presence of lead shielding [8].
For gynecologic cancer, Karol et al. [9] presented the three-dimensional image-based planning for cervix HDR brachytherapy for cervical cancer patients with bilateral metal hip prostheses using MVCT imaging in two patients. They concluded MVCT imaging eliminated streak artifacts, which improved the image quality of treatment planning. MVCT offers an option for three-dimensional planning for cervix brachytherapy in patients with bilateral hip prostheses. MVCT images provided adequate contrast to allow the contouring of OARs and the digitization of HDR applicators [9].
In dosimetric data, MVCT images had the enough details for use in volume-based approaches. Wagner et al. [10] reported using a commercially available helical tomotherapy treatment unit and standard low-dose rate (LDR) brachytherapy applicators used for treatment of cervical carcinoma. The D2cc of the bladder and rectum were computed from dose-volume histograms and compared to the doses computed for the standard ICRU bladder and rectal reference dose points. Fifteen brachytherapy insertions were analyzed. The ICRU rectal point dose did not differ significantly from rectal D2cc (p = 0.749; mean difference, 24 cGy +/- 283 cGy). The ICRU bladder point dose was significantly lower than the bladder D2cc (p = 0.024; mean difference, 291 cGy +/- 444 cGy). This initial experience in using MVCT imaging for clinical LDR gynecological brachytherapy indicates that the MVCT images are of sufficient quality for use in 3D, MVCT-based dose planning [10].
Our report showed the same idea using of MVCT in gynecologic brachytherapy. MVCT reduced the streak artifact causing by metallic applicator that tempered the treatment planning in brachytherapy and provided enough image quality to contouring. It allowed us to optimize the dose distributions to target and OARs. However, the limitation is that the image of MVCT is not clear in soft tissue differentiation as kVCT. In the complicated case as downward movements of small bowels, the contouring of HR-CTV, bladder, rectum and sigmoid is harder. In our institute, according to our infrastructure defect (CT simulator has broken), the use of MVCT for brachytherapy is an option to provide IGBT to our patients. The details of target and organs at risk were defined and the volume-based planning could perform to get benefit to the patient.
Acknowledgments
The author offers many thanks to the NRU-CMU in the Gynecologic Oncology Cluster, the Research Unit of Faculty of Medicine, Chiang Mai University. Definitely, the author conveys many thanks to our staff at the Division of Therapeutic Radiology and Oncology, Faculty of Medicine, Chiang Mai University, for supporting this study.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.