Observational approach on regional lymph node in cutaneous melanomas of extremities
Article information
Abstract
Purpose
We evaluated failure pattern and treatment outcomes of observational approach on regional lymph node (LN) in cutaneous melanoma of extremities and sought to find clinico-pathologic factors related to LN metastases.Material and
Methods
We retrospectively reviewed 73 patients with cutaneous melanoma of extremities between 2005 and 2016. If preoperative 18-F-fluorodeoxyglucose (FDG)-positron emission tomography/computed tomography (PET/CT) findings were non-specific for regional LNs, surgical resection of primary tumors with adequate margins was performed without sentinel lymph node biopsy (SLNB) and/or complete lymph node dissection (CLND), irrespective of tumor thickness or size. In patients with suspicious or positive findings on PET/CT or CT, SLNB followed by CLND or CLND was performed at the discretion of the surgeon. We defined LN dissection (LND) as SLNB and/or CLND.
Results
With a median follow-up of 38 months (range, 6 to 138 months), the dominant pattern of failure was regional failure (17 of total 23 events, 74%) in the observation group (n = 56). Pathologic LN metastases were significant factor for poor regional failure-free survival (hazard ration [HR] = 3.21; 95% confidence interval [CI], 1.03–10.33; p = 0.044) and overall survival (HR = 3.62; 95% CI, 1.02–12.94; p = 0.047) in multivariate analysis. In subgroup analysis for cN0 patients according to the preoperative PET/CT findings, LND group showed the better trend of LRFFS (log rank test, p = 0.192) and RFFS (p = 0.310), although which is not statistically significant.
Conclusion
Observational approach on regional LNs on the basis of the PET/CT in patients with cutaneous melanoma of extremities showed the dominant regional failure pattern compared to upfront LND approach. To reveal regional lymph node status, SLND for cN0 patients may of importance in managing cutaneous melanoma patients.
Introduction
Melanoma is one of highly aggressive form of cancers originating from melanocytes. More than 95% of cases diagnosed are cutaneous melanoma [1]. In South Korea, age standardized mortality rates of cutaneous melanoma are 0.23 per 100,000 for men and 0.16 per 100,000 for women, and it shows increasing trend between 1985 and 2003 [2]. Primary treatment of melanoma is surgical removal with an adequate resection margin [3] and it is important to assess the status of regional lymph node (LN) since melanomas often metastasis through regional lymphatic channels. Sentinel lymph node biopsy (SLNB) is the first-line approach for treating melanoma patients who have risk of regional LN metastasis, as SLNB is associated with fewer complications than complete lymph node dissection (CLND) [4]. SLNB is a minimally invasive technique, of which role and procedure are well-established in the Multicenter Selective Lymphadenectomy Trial (MSLT) I trial [5]. The American Society of Clinical Oncology and Society of Surgical Oncology recommend performing SLNB when Breslow thickness is between 1 to 4 mm. Based on National Comprehensive Cancer Network (NCCN) Guideline [6], SLNB is considered when tumor thickness ranged from 0.76 to 1 mm. Once a patient has positive SLN, CLND is strongly recommended although the benefit of overall survival is unclear [7]. Despite of recommendations from several guidelines [7,8], some clinicians still might prefer observational approach without LN dissection based on previous studies [9-11] due to possible complications, especially when initial imaging studies such as magnetic resonance imaging or 18-F-fluorodeoxyglucose (FDG)-positron emission tomography/computed tomography (PET/CT) show no metastatic finding.
The purpose of the present study is to analyze outcomes of observational strategy on regional LNs in our institution and to determine factors associated with treatment failure. Patterns of failure were identified, and we investigated clinical or pathologic factors relate to regional LN metastases.
Materials and Methods
1. Study participants
The present study was approved by Institutional Review Board at Seoul National University Hospital (IRB No. B-1604/343-114) and the informed consent was waived. Medical records of patients who had been diagnosed of cutaneous melanoma in extremities at Seoul National University Bundang Hospital between 2005 and 2016 were retrospectively reviewed. Patients were excluded from the study if they had melanoma in situ or had distant metastatic disease at the time of diagnosis. Additionally, one patient who did not have information of the the preoperative PET/CT were excluded. Seventy-three patients with median age of 60 years (range, 11 to 90 years) were included in the present study. Thirty were males and 43 females with Eastern Cooperative Oncology Group performance status 0 or 1. The primary site located in upper extremities in 19 patients (26.0%) and lower in 54 (74.0%), respectively.
2. Treatment
Presence of regional LN metastases were suspected if they showed more intense uptake in regional LN basin distant from the primary tumor compared with soft tissue. In most patients, if the preoperative PET/CT findings were non-specific for regional LNs, surgical resection of primary tumors with adequate margins was performed without SLNB or CLND irrespective of tumor thickness or size. In all patients with suspicious or metastatic LN findings from the preoperative PET/CT, SLNB and/or CLND was performed at the discretion of treating surgeon. LN dissection (LND) group (n = 16) was defined as patients who had underwent SLND and/or CLND. Fifty-seven patients were on observation and 8 with cN0 underwent LND, presumably at the discretion of the surgeon. The median number of harvested LNs and positive LNs were 6 (range, 1 to 29) and 2 (range, 1 to 10), respectively.
Adjuvant interferon-alpha (INF-α) was administered for 1 year when a patient had melanomas which thickness >4 mm in depth (stage IIB), or LNs metastases and was medically feasible. Only one patient in LND group were treated with postoperative radiotherapy owing to extra-capsular extension of involved LNs. Six patients received radiotherapy after salvage surgery for regional LN failures. Postoperative radiotherapy after salvage LND was initiated within 4 weeks of LND. The dose was 50 Gy given in 20 fractions over 4 weeks, except for one patient (52 Gy with unknown fractions at another hospital). The planned target volume encompassed dissected LN regions, and radiation was delivered using photons or electrons.
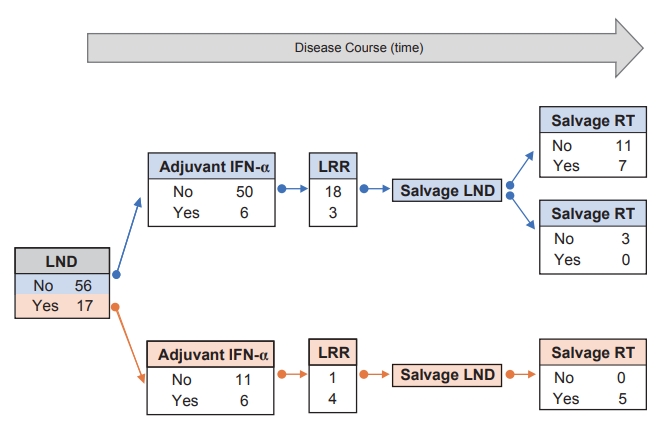
The flow of treatment scheme for study subjects and their number in each step are represented in Fig. 1.
3. Statistical analysis
Clinico-pathologic factors were identified and compared between two groups using chi-square test if needed. Survival rates including 2-year locoregional failure-free survival (LRFFS), regional failure-free survival (RFFS), distant metastasis-free survival (DMFS), and overall survival (OS) were estimated by the Kaplan-Meier method and compared with log-rank test. Also, Kaplan-Meier curves were depicted to compare between the LND and the observation group. In multivariate analysis, the Cox proportional-hazards regression models were established using factors with an estimated p-value less than 0.05 from univariate analysis.
All tests were two tailed, and p-value less than 0.05 was considered significant. Statistical analyses were performed using STATA software version 14.0 (Stata Corporation, College Station, TX, USA).
Results
1. Clinical and pathologic characteristics
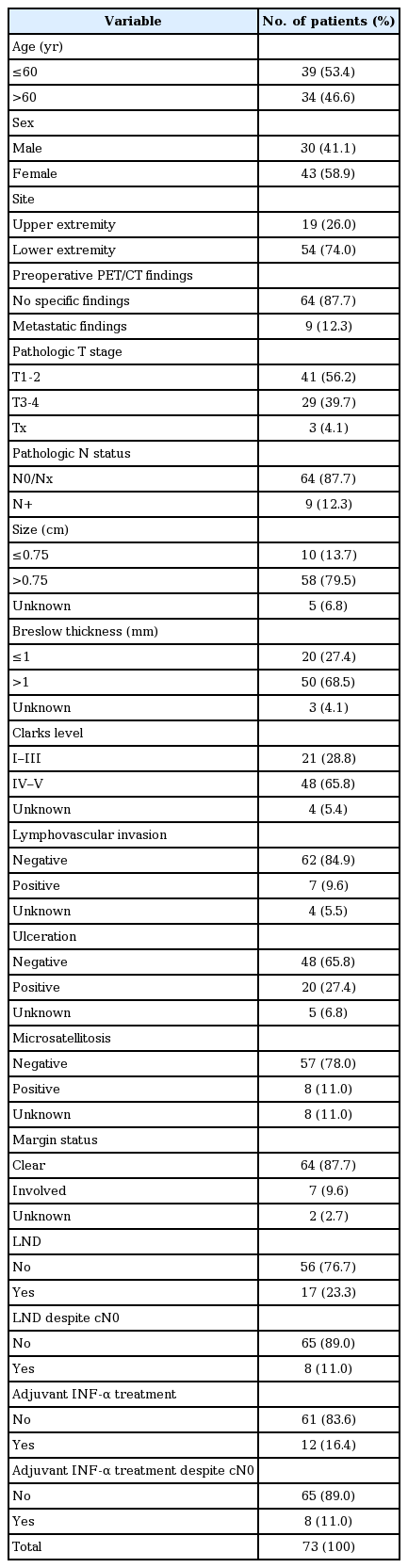
Table 1 shows the clinical and pathologic characteristics of patients. Fifty-four patients (74%) had cutaneous melanoma in lower extremity. Patients were treated with primary resection with LND (n = 17; 23.3%) or with observation (n = 56; 76.7%). Fifty patients (68.5%) demonstrated lesions of the Breslow thickness more than 1 mm, and 48 patients (65.8%) showed the lesions of the Clarks level of IV or V. Lesions which were more than 0.75 cm were found in 58 patients (79.5%). Nine patients (12.3%) represented metastatic findings at regional nodes initially from PET/CT findings, who were all treated with primary resection with LND.
Among LND group (n = 17), 9 patients had pN+ and 8 patients demonstrated pN0. The median harvested LNs in the LND group was 7 (range, 1 to 29). According to the preoperative PET/CT findings, only 1 of 8 patients with cN0 turned out to be pN+. Conversely, 1 of 10 patients were cN+ revealed pN0 (Supplementary Table S1).
2. Patterns of failure and clinical outcomes
Patterns of failure are represented in Fig. 2A. With median follow-up of 38 months (range, 6 to 138 months), the most dominant pattern of failure in all patients was the regional failure (22 of total 31 events, 71%). The proportion of regional failure in the observation group was 74% (17 of total 23 events), and that of regional failure in the LND group was 63% (5 of total 8 events). LND group had distant failure as a dominant failure pattern (7 of 8 events, 88%). Relative failure frequency between groups is shown in Fig. 2B. Locoregional recurrences were more frequently identified in the observation group than LND group (75.0% vs. 41.7%). Conversely, the incidence of distant metastases was higher in the LND group rather than the observation group (58.3% vs. 25.0%).

(A) The number of failure events in the overall, observation, and LND group are represented via the Venn diagram. Numbers in parentheses are the number of patients in the group. (B) Percentage of failure events in the observation versus the LND group is represented in the bar graph. LND, lymph node dissection
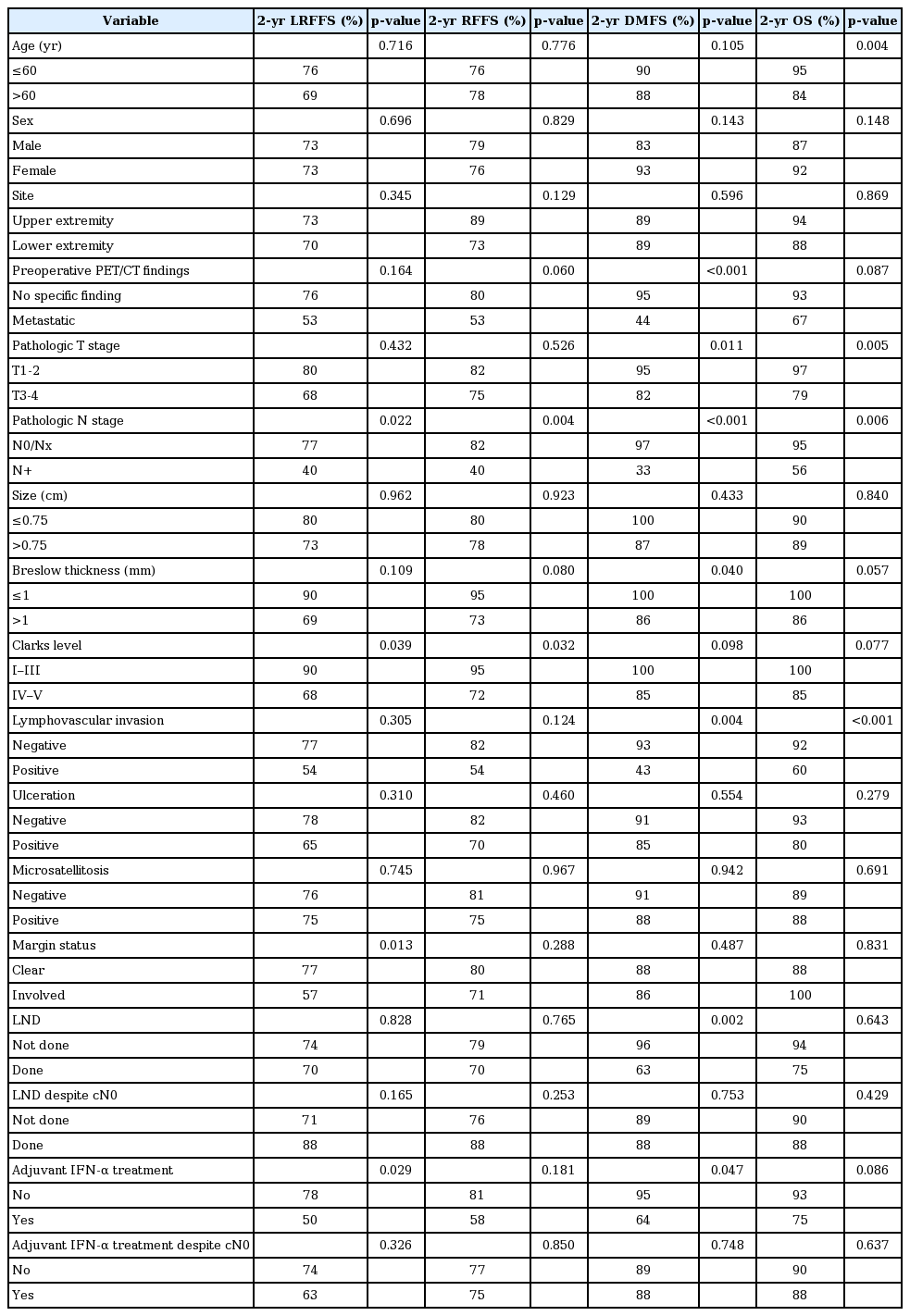
Table 2 shows results of univariate analysis for survivals. Compared to patients with pN0/pNx, those with pathologically positive LN (pN+) has significantly worse 2-year LRFFS (40% vs. 77%, p = 0.022), 2-year RFFS (40% vs. 82%, p < 0.004), 2-year DMFS (33% vs. 97%, p < 0.001), and 2-year OS (56% vs. 95%, p = 0.006) rates. Metastatic findings in the preoperative PET/CT findings were significantly associated with worse DMFS (44% vs. 95%, p < 0.001). Involved margin was associated with poorer LRFFS (57% vs. 77%, p = 0.013) and PFS (43% vs. 76%, p = 0.001), but not DMFS and OS. The presence of lymphovascular invasion (LVI) is the poor prognostic factor associated with DMFS (43% vs. 93%, p = 0.004) and OS (60% vs. 92%, p < 0.001). LND was associated with lower DMFS than observation group (63% vs. 96%, p = 0.002).
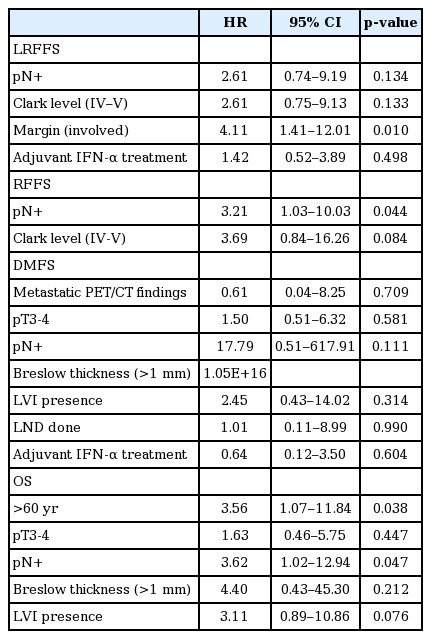
In multivariate analyses (Table 3), involved margin status was an independent prognostic factor for LRFFS (hazard ratio [HR] = 4.11; 95% confidence interval [CI], 1.41–12.01; p = 0.010). pN+ was independently associated with poor RFFS (HR = 3.21; 95% CI, 1.03–10.03; p = 0.044) and OS (HR = 3.62; 95% CI, 1.02–12.94; p = 0.047). Age more than 60 years was detrimental factor for OS as well (HR = 3.56; 95% CI, 1.07–11.84; p = 0.038).
For subgroup analysis, we next compared the survivals between the LND and the observation group who showed cN0 from the preoperative PET/CT findings. No statistically significant differences between groups were found in LRFFS, RFFS, DMFS, and OS. However, trends of better 3-year LRFFS (88% vs. 71% in Fig. 3A) and RFFS (88% vs. 77% in Fig. 3B) are observed in the LND group compared with the observation group. However, 3-year DMFS and OS were similar between groups (Fig. 3C and 3D).

As a subgroup analysis, Kaplan-Meier curves comparing survivals between the LND (n = 56) and the observation group (n = 8) who did not show the initial metastatic findings in PET/CT (cN0, total n = 64): (A) locoregional failure-free survival, (B) regional failurefree survival, (C) distant matastasis-free survival, and (D) overall survival. p-values were estimated from log-rank test. LND, lymph node dissection.
Factors associated with pN+ were presented in Supplementary Table S1. Metastatic findings of the preoperative PET/CT were more frequent in patient with pN+ than those with pN0 (88.9% vs. 12.5%; p = 0.002). The sensitivity, specificity, positive and negative predictive value of PET/CT predicting pN+ were 88.9%, 87.5%, 88.9% and 87.5%, respectively. Although distribution of pathologic findings such as the Clark level, ulceration, the presence of LVI or microsatellitosis were not significantly different between the pN0 and pN+ groups, the trend of enriched favorable factors in patients with pN0 was observed.
Discussion and Conclusion
Despite SLNB is regarded as the part of the standard approach to cutaneous melanoma [8], SLNB for all cutaneous melanoma patients have been questionable [9-11]. Current study shows that regional LN metastasis was the dominant failure pattern in the observation group compared with the LND group. We found that pN+ had detrimental effect on RFFS, DMFS, and OS. To manifest the pathologic LN status, performing LND may be important practice in addition to the preoperative PET/CT findings.
Pathologic LN involvement is independently associated with survivals, and some risk factors for pN+ were identified in previous studies: thickness, Clarks level, ulceration, and mitotic rate. Thickness of melanomas is associated with pathologic LN positivity. Meta-analysis from 60 studies (10,928 patients) demonstrated that SLN positivity was 4.5% for thin melanoma (≤1.0 mm), but a likelihood of SLN metastases was soared up to 8.8% when thickness was equal to or greater than 0.75 mm [12]. A large retrospective review from the SLN Working Group of 1,250 patients with thin melanoma revealed that in melanoma patients with Breslow thickness ≥0.75 mm, the predicted SLN positivity is 6.3%. Clark level ≥IV and ulceration for thin melanoma were associated with SLN positivity in 7.0% and 11.6% of cases, respectively [13]. As for mitosis, Mozzillo et al. [14] reported that mitotic rate is the only prognostic factor to SLN positivity for thin melanoma. Aligned with previous studies, current study found that Breslow thickness, Clarks level, margin status, and LND were marginally associated with LRFFS in whom with no metastatic findings in the the preoperative PET/CT.
PET/CT is used to detect clinically regional or distant metastasis in various types of cancers. Unfortunately, there is no clinical trial to determine the role of PET/CT for the staging of melanoma to date. Although, a systemic review [15] concluded that PET/CT had higher sensitivity and specificity for AJCC stages III and IV melanoma patients, authors of the review did not agree with the broad use of PET/CT for primary staging due to the wide ranges of sensitivity and specificity of PET/CT. There is a study even reporting the sensitivity of 0% (95% CI, 0%–23%) of FDG-PET scan in detecting metastatic disease in patients with primary cutaneous melanomas of Breslow thickness 1 mm or greater [16]. Conversely, Rinne et al. [17] showed that PET had 100% of sensitivity and 94% of specificity in detecting LN metastases for the thick melanoma (>1.5 mm), suggesting practical role of PET as staging modality. In current study, sensitivity of the preoperative PET/CT for detecting metastatic LN was 88.9%, and this favors additional surgical approaches such as SLND and/or CLND for predicting metastatic LNs.
Our interest was that there is a role of LND in patients even without clinical evidence of regional LN metastasis in initial imaging studies. We found that performing LND in those without metastatic findings from the preoperative PET/CT showed the trend of better 3-year LRFFS and RFFS, although which was not statistically significant. Ten-year results from the MSLT-I trial [5] showed a significant difference in disease-free survival (DFS) between the SLN biopsy and the observation groups for patients with intermediate to thick melanomas defined as ≥1.2 mm. Compared to MSLT-I trial, we showed the 3-year RFFS of 77% in cN0 group, which is comparable to the 3-year DFS in cN0 patients with intermediate-thickness melanoma reported from MSLT-I trial. However, it is hard to directly compare between two studies due to the discrepancies of the design of study, follow-up duration, or adjustment of covariates. As another retrospective series supporting SLNB, Ribero et al. [18] showed that in 350 patients with thick melanomas >4 mm, better disease-free interval in the SLNB group than the observation group (HR = 0.59; 95% CI, 0.43–0.79; p = 0.001) was observed. Another retrospective study reported no difference in melanoma-specific survival, but significant improvement in DFS, regional recurrence-free survival, and DMFS in the SLNB group, addressing the benefit of the SLNB [11].
SLNB offers several benefits in patients with high-risk of regional LN metastasis. SLNB can identify patients with LN metastases and avoid elective LN dissection. Whether regional LN is involved or not is important to predict prognosis [19] and the information about the status of regional nodes can help select patients who may benefit from adjuvant therapy such as radiation therapy or chemotherapy [5]. Detection of SLN involvement can leads to an early decision of CLND. Subgroup analysis of MSLT-I trial [20] reported that early CLND based on the result of SLNB is associated with reduced incidence and severity of lymphedema compared with delayed CLND. False negative rate of SLNB is likely to be lower than that of CLND because pathologists can examine a few LNs thoroughly.
There are some limitations in our study. As a retrospective review of a single-institution with small number of patients, selection bias could potentially affect our results, particularly in deciding LND. Another limitation is that decision making between SLND and CLND was at the discretion of treating surgeon and it was difficult to investigate the different role between SLND and CLND.
In conclusion, the present study found that regional failure was the dominant failure pattern in the observation group compared with the LND group. Pathologic regional LN metastasis was associated with decreased survival. In addition to preoperative PET/CT imaging, SLND may be recommended with primary resection to uncover the status of regional LN.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Supplementary Materials
Supplementary materials can be found via https://doi.org/10.3857/roj.2018.00507
Table S1. Clinicopathologic characteristics between pN0 and pN+ patients.