Evaluation of the heart and lung dosimetric parameters in deep inspiration breath hold using 3D Slicer
Article information
Abstract
Purpose
The present study was conducted to compare dosimetric parameters for the heart and left lung between free breathing (FB) and deep inspiration breath hold (DIBH) and determine the most important potential factors associated with increasing the lung dose for left-sided breast radiotherapy using image analysis with 3D Slicer software.
Materials and Methods
Computed tomography-simulation scans in FB and DIBH were obtained from 17 patients with left-sided breast cancer. After contouring, three-dimensional conformal plans were generated for them. The prescribed dose was 50 Gy to the clinical target volume. In addition to the dosimetric parameters, the irradiated volumes and both displacement magnitudes and vectors for the heart and left lung were assessed using 3D Slicer software.
Results
The average of the heart mean dose (Dmean) decreased from 5.97 to 3.83 Gy and V25 from 7.60% to 3.29% using DIBH (p < 0.001). Furthermore, the average of Dmean for the left lung was changed from 8.67 to 8.95 Gy (p = 0.389) and V20 from 14.84% to 15.44% (p = 0.387). Both of the absolute and relative irradiated heart volumes decreased from 42.12 to 15.82 mL and 8.16% to 3.17%, respectively (p < 0.001); however, these parameters for the left lung increased from 124.32 to 223.27 mL (p < 0.001) and 13.33% to 13.99% (p = 0.350). In addition, the average of heart and left lung displacement magnitudes were calculated at 7.32 and 20.91 mm, respectively.
Conclusion
The DIBH is an effective technique in the reduction of the heart dose for tangentially treated left sided-breast cancer patients, without a detrimental effect on the left lung.
Introduction
Radiotherapy after breast-conserving surgery removes microscopic disease in the conserved breast; therefore, it diminishes the risk of local recurrence and distant metastasis among patients. As a result, it improves the survival rate among them [1]. However, despite its benefit in the reduction of cancer-specific mortality, radiotherapy is known to cause cardiovascular disease and lung cancer, especially in patients with left-sided breast cancer [2,3]. The rate of ischemic heart disease increases linearly by 7.4% for each increase of 1 Gy in the mean heart dose [4]. As there is no threshold dose below which the side effects cannot occur; therefore, in recent years, there has been a lot of efforts to decrease the delivered dose to the organ at risks (OARs) as much as possible [2,4-6].
Deep inspiration breath hold (DIBH) is one of the methods used for the above-mentioned purpose. It is a simple and effective technique in decreasing the heart dose without compromising the coverage of target volume in patients with left-sided breast cancer [5]. In DIBH, the heart simply moves posteriorly and inferiorly due to lung expansion and diaphragmatic movement; as a result, the distance between the heart and irradiated areas, such as the breast and chest, increased leading to a reduction in the irradiated heart volume and its dose [2,7,8]. Although this technique reduces the heart dose [7-12], it seems that there are challenges in the reduction of lung dose with DIBH [13]. Despite the results of many studies showing the reduction of the ipsilateral lung dose [2,7,11,14], there are reports of no significant difference and even increasing the left lung dosimetric parameters using DIBH [8,15-20].
Therefore, the primary aim of this study was to compare the dosimetric parameters of the heart and left lung between free breathing (FB) and DIBH. In the second place, the present study determined the most important potential factors associated with increasing the lung dose in left-sided breast radiotherapy with the calculation of various parameters, such as the irradiated volume and displacement of the lung, during DIBH in patients with left-sided breast cancer using image analysis with 3D Slicer software (version 4.10.1, Brigham and Women’s Hospital, Boston, MA, USA) [21].
Materials and Methods
1. Patient selection
This study was carried out on 17 patients with early left-sided breast cancer who referred for postoperative radiotherapy following undergoing breast-conserving surgery during 2017–2019. The subjects enrolled in the present study voluntarily and signed the informed consent before the computed tomography (CT) simulation. These patients should be capable of holding their breath for at least 20 seconds.
This study was approved by the Institutional Review Board of Mashhad University of Medical Sciences (No. 970830).
2. CT scan
In the CT simulation, two scans were acquired with 5 mm slice thickness that was the first scan in FB and another in the DIBH state. The patients were scanned in the supine position using a breast board while their left arm was placed above the head. To perform DIBH, a novel system was used as a house respiratory gating system [22]. This system uses the CD22-100AM122 distance meter laser sensor. The laser was adjusted between the xiphoid process and umbilicus at a distance of 10 cm to the body surface. This distance is changed by respiration, and then, these changes are detected in the output of the sensor. As a result, the respiratory signal is displayed on the monitor. Firstly, the patient was requested to breathe in and out and then breathe deeply. When a stable deep inspiration level was acquired, the upper and lower thresholds were placed on the respiratory signal for the determination of the gating window. Moreover, the gating window was adjusted to 5 mm. Finally, the patient was asked to breathe deeply and put the respiratory signal in the gating window and keep it for approximately 20 seconds; therefore, the CT image was acquired at this time.
3. Treatment planning
The clinical target volume (CTV) and OARs, including the heart and left lung, were contoured by an oncologist. The prescribed dose was 50 Gy in 2 Gy daily fractions to the CTV. It was delivered by the three-dimensional conformal technique with two opposing 6 MV tangential fields and additional subfields. In the treatment planning, at least 95% of the CTV should be covered by the 95% isodose lines. In addition, hotspots up to 107% of the prescribed dose were acceptable. After planning, central lung distance (CLD) and lung length (LL) were calculated in the medial field. The CLD refers to the distance between the edge of the lung contour and tangential field border in the central axis on a digitally reconstructed radiograph; however, LL refers to the vertical distance of the lung, which is vertically placed in the radiation port [23].
4. Image analysis
In the current study, 3D Slicer software (version 4.10.1) was used for the calculation of the parameters, including the irradiated heart and left lung volumes, as well as the displacement values, for them during DIBH.
5. Irradiated volumes of heart and left lung
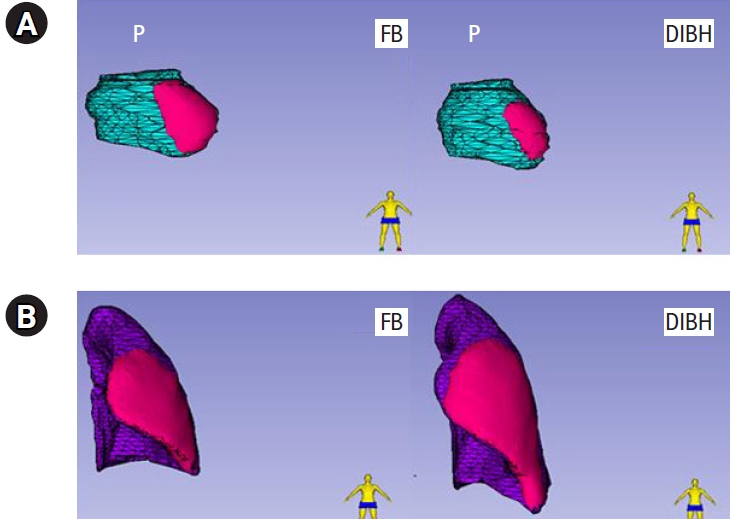
In this study, the absolute and relative irradiated volumes for the heart and left lung were calculated for FB and DIBH separately. For instance, the method of the calculation of the irradiated left lung volume in DIBH was completely described as it follows.
For this purpose, the CT image, RT Structure, and RT Plan were loaded into the software platform. Then, the Segmentation module was used for the creation of the left lung model. After that, the lung model and radiation fields were imported into the segmentation created by the segmentation module.
The intersection between the left lung model and each of the radiation fields were obtained by the Segment Editor module. The irradiated volumes in the medial and lateral fields were added together by which the total left lung volume was acquired in the radiation fields. Finally, the Segment Statistics module was used for the calculation of the numerical value of this irradiated volume. In addition, to estimate the relative irradiated volume, the absolute irradiated volume was divided into the total volume. As shown in Fig. 1, the irradiated volumes of the heart and left lung were calculated in the FB and DIBH states.
6. Calculation of displacements for heart and left lung during DIBH
In the present study, the numerical values of the displacement were calculated for the heart and left lung between two FB and DIBH states. For instance, the methods of calculating the magnitude of the left lung displacement and displacement vectors in different directions (i.e., anterior-posterior [AP], right-left [RL], and superior-inferior [SI]) were completely described as it follows.
1) Magnitude of displacement
Firstly, the CT images and RT Structures were loaded into the software platform. After that, the Segmentation module was used for the creation of the left lung models for FB and DIBH separately. For the calculation of the displacement field, the left lung models had to be registered between the FB and DIBH states using the Segment Registration module. Following that, all displacement magnitudes were obtained by the Transforms module. Finally, the Segment Statistics module was used for the calculation of the average value of displacement magnitudes.
2) Displacement vectors in SI, AP, and RL directions
For obtaining the displacement vectors in the AP, RL, and SI directions, the left lung models were registered as before. After that, the deformable left lung was imported into the segmentation created by the Segmentations module. The out regions of the left lung should be blanked to have the displacement vectors only in the deformable left lung. For this purpose, the Segment Editor module was used in this study. The result of this step was displacement vectors only for the deformable left lung renamed to the masked displacement field. The masked displacement field was saved and then extracted its components in the AP, RL, and SI directions by a self-written program in Python programming language followed by the calculation of their mean values in any directions. Furthermore, the differences between the parameters in DIBH and FB plans were calculated for each patient. These differences (ΔX) were calculated at XDIBH – XFB. After that, ΔX was normalized to the XFB that resulted in Δ'X and expressed as percentage.
7. Statistical analysis
A comparison between the parameters for FB and DIBH plans was performed using a paired sample t-test in SPSS version 22.0 (SPSS IBM, Armonk, New York, USA). These parameters included the Dmean, V20, V25, Vabs, Vrel, CLD, and LL. In addition, Pearson correlation coefficient was used to determine the correlation between the left lung Δ'Dmean with the Δ'Vabs, Δ'Vrel, Δ'CLD, and Δ'LL. p-value less than 0.05 was considered statistically significant. Finally, the average of mean displacement magnitudes, as well as vectors in SI, AP, and RL directions, were calculated in this study.
Results
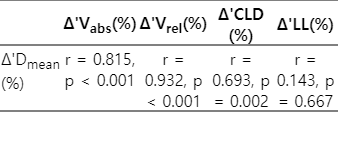
As shown in Table 1, DIBH was associated with a significant reduction in the heart dosimetric parameters (p < 0.001); however, there was no statistically significant difference in the left lung dosimetric parameters (p > 0.05). The average of the heart Dmean reduced from 5.97 to 3.83 Gy with DIBH. Similarly, the mean of V25 decreased from 7.60% to 3.29%. The average of left lung Dmean was changed from 8.67 Gy (FB) to 8.95 Gy (DIBH). In addition, the mean of V20 was obtained 14.84% with FB and 15.44% by DIBH. The average of CLD significantly increased from 2.18 to 2.47 cm with DIBH (p < 0.001). Moreover, LL significantly increased from 14.12 cm for FB to 18.05 cm for DIBH (p < 0.001).
Comparison of dosimetric parameters, CLD, and LL between FB and DIBH plans in patients with left-sided breast cancer
1. Irradiated volumes of heart and left lung
The results of Table 1 show that the mean of heart Vabs significantly decreased from 42.12 to 15.82 mL using DIBH (p < 0.001). Similarly, heart Vrel decreased from 8.16% to 3.17% (p < 0.001). For the left lung, Vabs significantly increased from 124.32 mL with FB to 223.27 mL by DIBH (p < 0.001). Furthermore, Vrel was changed from 13.33% with FB to 13.99% by DIBH (p > 0.05). As shown in Table 2, there was a significant correlation between Δ'D with both of the Δ'Vabs and Δ'Vrel. Moreover, the correlation between the Δ'D and Δ'CLD was significant (p = 0.002); however, the correlation between Δ'D and Δ'LL was not significant (p = 0.667).
2. Displacements for heart and left lung during DIBH
As shown in Table 3, the average of mean displacement magnitude for the heart was 7.32 mm. In addition, the maximum value for the mean of heart displacement vectors was in the inferior direction. The average of the mean displacement magnitude for the left lung was 20.91 mm. Moreover, the maximum values for the mean of left lung displacement were in the SI directions.
Discussion and Conclusion
The results of the present study demonstrated the ability of DIBH in the reduction of the heart dose in patients with left-sided breast cancer as reported in previous studies [7-12]. However, similar to some reports, the collected data of the present study did not show the protective effect of this technique on the left lung [8,15-20]. In the present study, the average of the heart Dmean and V25 significantly decreased using DIBH. Also, the absolute and relative irradiated volumes of the heart significantly decreased by this technique. In DIBH, the left lung expansions in different directions pushed the heart away from the radiation fields and irradiated areas that is the most important reason for the reduction of irradiated heart volume and dose.
Jensen et al. [24] reported that the average of the heart Dmean decreased from 3 Gy with FB to 2 Gy by DIBH. In addition, they observed that the average of the heart V25 decreased from 3.3% (FB) to 1.0% (DIBH). Sung et al. [25] demonstrated that the average of the heart Dmean decreased from 5.9 Gy with FB to 3 Gy in DIBH.
Hayden et al. [8] reported that the irradiated heart volumes were 36.9 mL (FB) and 2.1 mL (DIBH), which were smaller than the results of the present study. In addition, in a study carried out by Sung et al. [25], the irradiated heart volumes were reported as 41.7 and 12 mL for FB and DIBH, respectively, which were almost consistent with the findings of the present study. The differences between contouring and patient anatomy lead to higher dosimetric parameters of the heart, compared to those in other studies. The smaller lung volume in Asian women in comparison to that in non-Asians might lead to a lower distance between the left ventricle and chest wall, which explains the higher irradiated heart volume in this study [7,26].
The maximum value for the mean of heart displacement vectors was in the inferior direction due to lung inflation and diaphragmatic movement that results in the greatest heart displacements in this direction.
Although the results of previous studies have shown that the mean heart dose reduces with DIBH [7-12], there are still some discrepancies in the left lung dosimetric parameters using this technique. In some studies, it was demonstrated that lung Dmean significantly reduced with DIBH [2,7,11,14]. However, in some studies, the lung dose was not significantly changed or even increased [8,15-20]. In the present study, it was observed that using DIBH led to an increase in the lung dose for some patients.
The obtained results of the present study showed that the absolute and relative irradiated volumes of the left lung increased using DIBH; however, the increase of relative irradiated volume was not significant. Also, Sung et al. [25] demonstrated that the average of irradiated lung volume increased from 155.1 mL (FB) to 253.5 mL (DIBH). Although, the results of some studies have shown that in the DIBH technique, the relative irradiated volume decreases despite increasing the absolute irradiated lung volume [2,12], Nevertheless, the results of the present study revealed that the relative irradiated volume increased in some patients. This volume was higher in DIBH than that in FB in almost all patients of the present study whose lung dosimetric parameters increased with DIBH. Therefore, it is expected to increase the dosimetric parameters of the left lung, if the relative irradiated volume increases.
Overall, discrepancies in the left lung dosimetric parameters among the studies are related to various factors, such as differences in the patient anatomy, contouring, treatment planning, and treatment methods.
The CLD is a parameter that can be used for the prediction of the irradiated lung volume in the tangential fields. The CLDs of 1.5, 2.5, and 3.5 cm can approximately predict 6%, 16%, and 26% of the ipsilateral lung, respectively, that would be included in the tangential fields [27]. The results of the patients in the present study were almost consistent with these values. Furthermore, the average of mean displacement of left lung magnitude in the present study was 20.91 mm. In addition, the maximum values of the mean displacement were acquired in SI directions and following that anterior direction.
In a study conducted by Oechsner et al. [28], the mean of displacement magnitude for the left lung was reported as 20.80 mm. Moreover, they calculated the mean of displacement in three directions, including left (1.5 mm), anterior (16.0 mm), and inferior (12.2 mm). According to the results of the present study and collected data, the averages of the left lung displacement magnitude in the two studies are completely similar. Nevertheless, in the aforementioned study, the anterior displacement is greater than the other two directions. However, in the present study, the maximum values of the mean displacement vectors were acquired in the superior and inferior directions and after that in the anterior direction. Their patients were trained to do chest breathing, although the patients in the present study were not trained to perform specific breathing that is an important reason for differences between the results of the two studies.
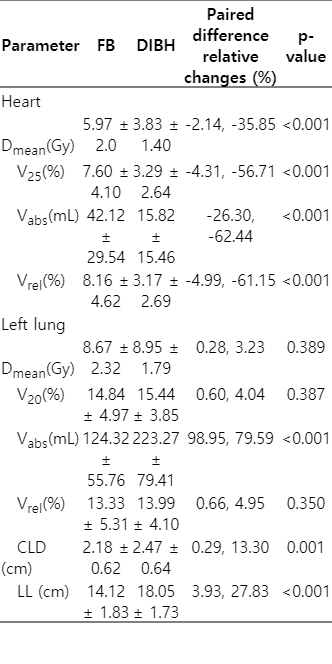
According to the potential factors that result in the increased left lung dosimetric parameters using DIBH, it seems that lung displacement into the irradiated areas is the most important factor. As shown in Fig. 2, the anterior displacement of the lung had the greatest effect on displacement toward the CTV. In addition, while performing DIBH, the parts of the lung outside the radiation field are placed in the field, as shown in Fig. 3. When the left lung moves toward the radiation fields, the absolute irradiated volume, as well as, the relative irradiated volume, increased, which resulted in an increase in the lung dosimetric parameters.
Representation of displacement vectors for one of the patients with increasing left lung dosimetric parameters during deep inspiration breath hold: (A) axial, (B) sagittal, and (C) coronal.
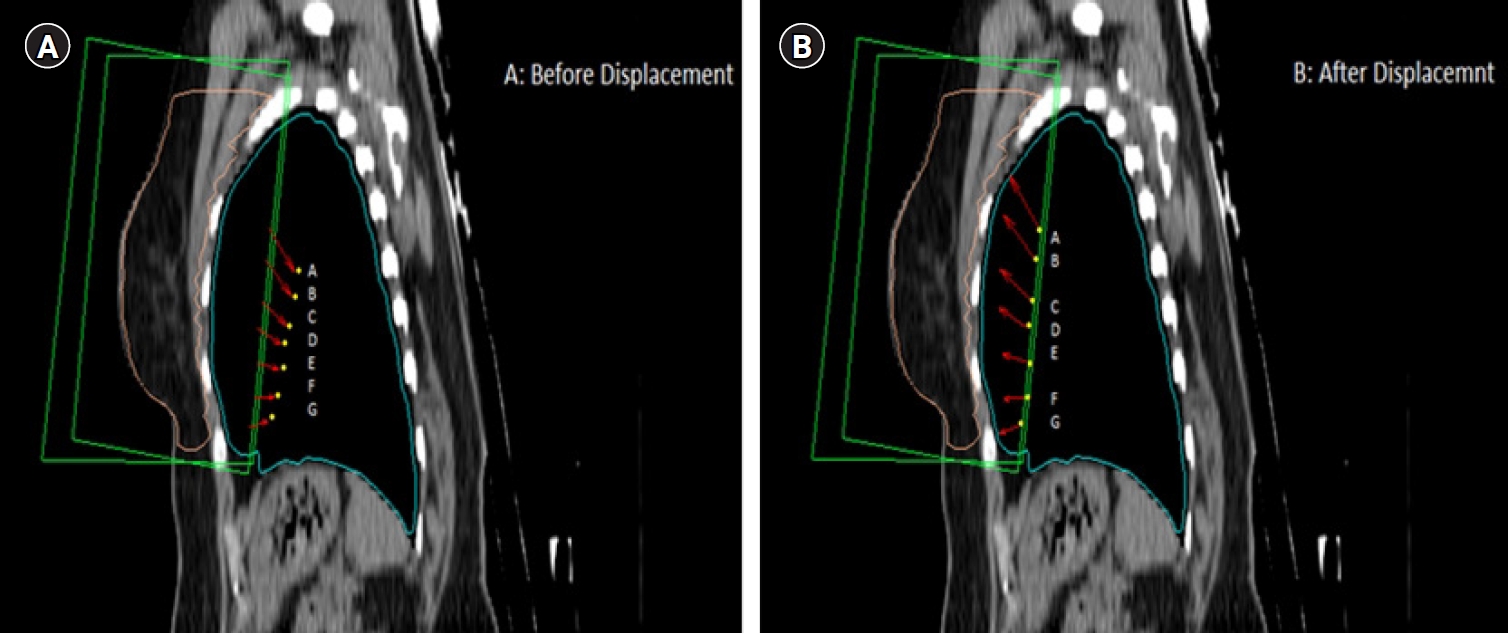
The A–G point positions of the left the lung relative to the radiation fields: (A) before displacement and (B) after displacement.
As shown in Table 2, by assessing the correlation of the lung Δ'D with other factors, such as Δ'Vabs, Δ'Vrel, Δ'CLD, and Δ´LL, there was a significant correlation between Δ'D with both Δ'Vabs and Δ'Vrel. The lung dosimetric parameters, such as Dmean and V20, can increase by rising the irradiated lung volume, especially Vrel. Moreover, there was a significant correlation between Δ'D and Δ'CLD. As previously mentioned, CLD is associated with irradiated lung volume. The increase in the CLD leads to an increase in lung Vabs and consequently Vrel for some patients. Therefore, lung Dmean increased in these cases. However, the significant correlation was not observed between Δ'D and Δ'LL. It is argued that among some patients in the present study, the left lung cranio-caudal movement had no significant effect on their dose reduction, and the anterior displacement was a more important factor in lung dose. Even in some of them, the upward and downward movements were greater than the anterior ones.
In addition, special attention should be given to patient anatomy that can be considered an effective factor in lung dose. Factors such as breast size and CTV, which determine the size of the radiation fields, as well as the chest shape can be considered effective factors in the lung dose. As Chilukuri et al. [29] reported in their abstract that the mean of the lung V20 significantly decreased in patients with a curved chest wall (12% vs. 19%; p = 0.001); however, the mean of lung V20 was acquired 21% versus 22.3% in patients with a flat chest wall (p = 0.78). According to the heart and lung dosimetric parameters, they concluded that patients with a curved chest wall obtained a significant benefit from DIBH.
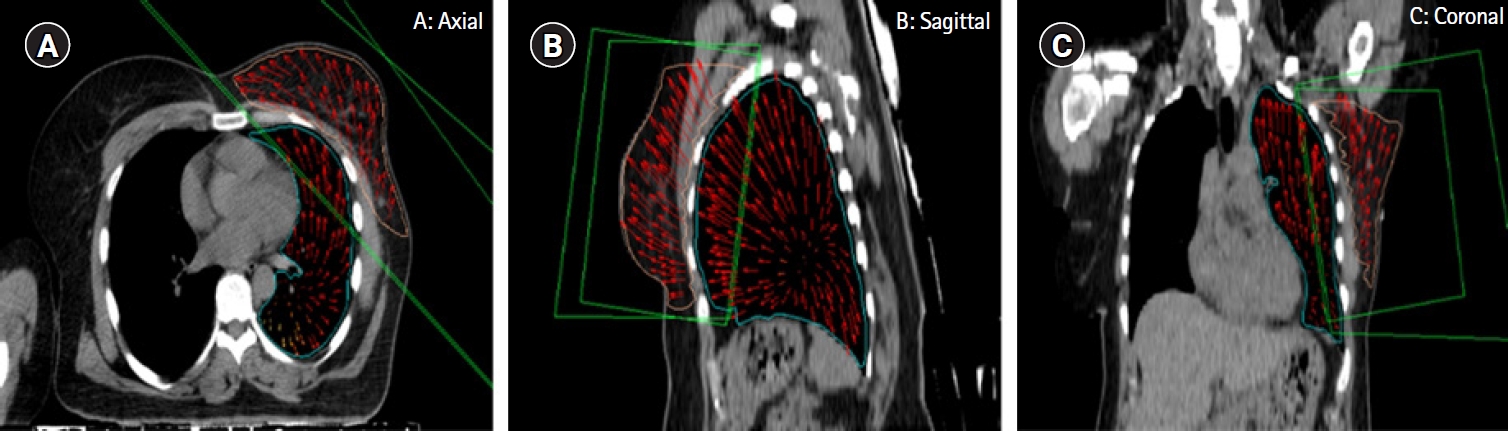
In general, with respect to the dosimetric parameters of the heart in the present study, all of the patients in this study could benefit from the DIBH technique, especially the subjects with large irradiated heart volume in the FB plan. Nevertheless, the results of the current study revealed that the DIBH technique did not necessarily decrease the lung dose. Based on the various factors, such as patient anatomy, including chest shape, breast size, direction of the lung displacements, as well as contouring and treatment planning, the lung dose can be varied in different patients, as shown in Fig. 4.
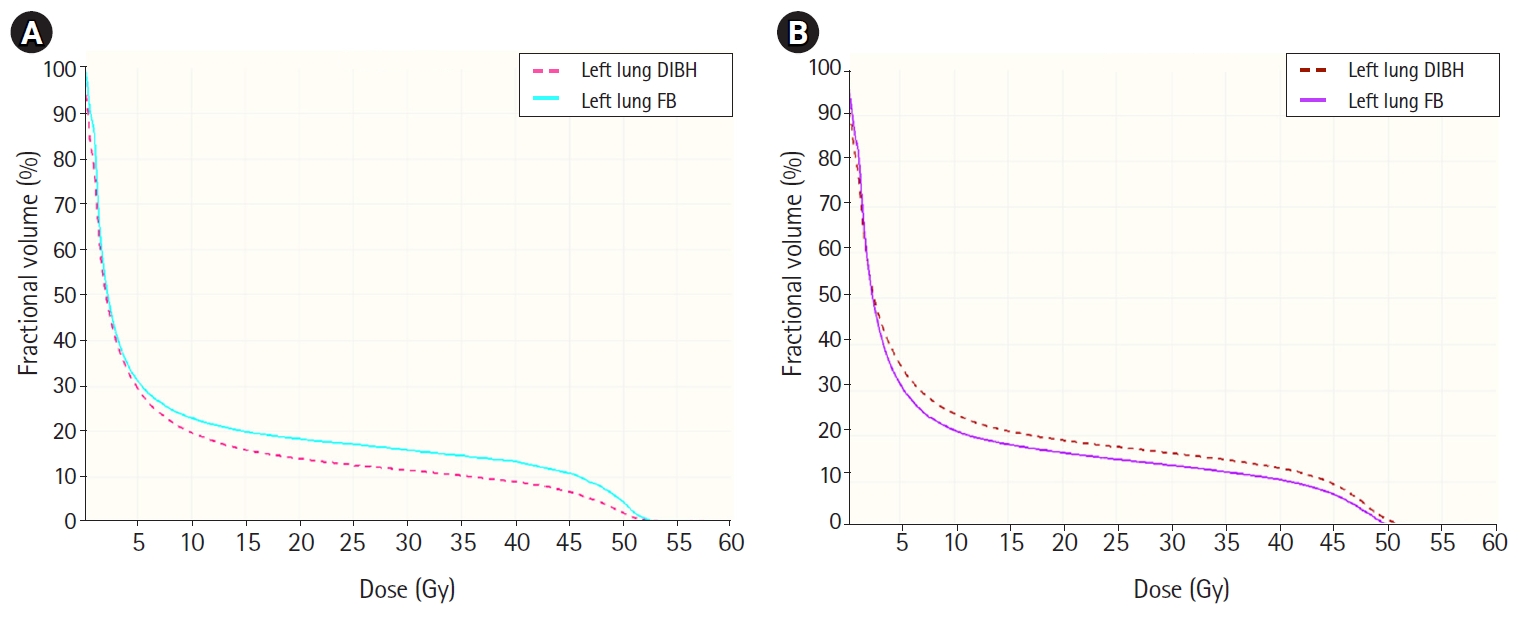
Left lung dose-volume histograms for 2 patients: (A) dose reduction and (B) increasing the lung dose by deep inspiration breath hold (DIBH). FB, free breathing.
Considering the heart dosimetric parameters, Joo et al. [7] reported that patients with long maximum heart distance (MHD) and small lung volume have highly benefited from this technique. However, it is required to perform further studies for the determination of the anatomical parameters that affect both the heart and lung dose reduction and lead to the selection of patients most likely to benefit from the DIBH technique.
Another strategy for the improvement of heart sparing in breast cancer treatment is intensity-modulated radiation therapy. In this technique, due to using more radiation fields, the normal volumes that occur in the radiation fields increase, which results in the increase of the normal tissue low-dose exposure. In addition, in this technique, due to the healthy tissues and CTV proximity, normal tissues occur in most radiation fields. Despite the reduction in the high-dose area, the low- and medium-dose regions in the heart and lung increase [2,30] that can raise the dosimetric parameters of OARs for some patients, as reported in some studies [31-34]. However, the high-dose regions in the heart could decrease without these additional increases in the low- and medium-dose areas using DIBH [2]. Nonetheless, the lung dose can be different in various patients with this technique.
As a result, in comparison to FB, DIBH is a more effective technique for the reduction of the heart dose, which is sometimes associated with increasing the left lung dosimetric parameters.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
The authors would like to thank the Research Vice-Chancellor of Mashhad University of Medical Sciences, Mashhad, Iran, for financial support from 970830 protocol code.