 |
 |
AbstractPurposeIntracavitary brachytherapy is one of the important methods of gynecological cancer treatment. The effect of attenuation is not considered in the dose calculation method released by the American Association of Physicists in Medicine Task Group No. 43 Report. In this study, the effect of high-dose rate brachytherapy applicators on dose distribution was measured using Gafchromic films and well-type ionization chamber.
Materials and MethodsA plan created by the treatment planning system was first executed using a well-type ionization chamber with a water equivalent elasto-gel in place for charge collection. Again, same plan was executed using central tandems of various angulations with different diameters of vaginal cylinders and charge collection was measured. For in vitro dose measurements this plan was also executed on tandem and vaginal cylinder assembly with Gafchromic films fixed on the surface of vaginal cylinder.
ResultsThe results show that the central tandem when used with different vaginal cylinders resulted in increase in effective attenuation of the beam. The central tandem of 300 angulations when used with a 35-mm diameter vaginal cylinder results in maximum attenuation whereas the 0º tandem when used with 20-mm diameter vaginal cylinder results in least attenuation of the beam.
ConclusionDue to the attenuation by various applicators used in brachytherapy for the treatment of gynecological cancers, it can be concluded that the difference between practical dose and the treatment planning system calculated dose should be considered for the correct estimation of the dose to the target and the organs-at-risk.
IntroductionBrachytherapy is one of the most important treatment modalities for gynecological cancers. The comprehensive global cancer statistics from the International Agency for Research on Cancer indicate that gynecological cancers accounted for 19% of the 5.1 million estimated new cancer cases in the world [1]. As per GLOBOCAN 2020 project data, breast cancer, cervical cancer, ovarian cancer, and uterine cancer are among the top-10 common cancers in females worldwide [2]. Gynecological cancers can be treated by various treatment modalities and the most common treatment modalities are surgery, radiation therapy, chemotherapy, and targeted therapy. Surgery is one of the treatment options for the early stage of cervical carcinoma other than local radiotherapy in the form of brachytherapy. However, the majority of patients present with either bulky or locally advanced diseases, so these patients are treated by concurrent chemoradiation with external beam radiotherapy followed by brachytherapy [3]. High-dose rate (HDR) brachytherapy was initially used for cervical cancers in many countries, but later on, it was integrated into treatment plans for vaginal cancers also [4].
In HDR brachytherapy, the dose optimization is done by the treatment planning system (TPS) to calculate the prescribed dose at the desired location and optimization is performed to reduce the dose to the nearby organs-at-risk (OAR). The prescribed dose is calculated by the TPS at desired location by varying the dwell times and dwell positions of a radioactive source along specified applicator paths. In intracavitary brachytherapy (ICBT) of cervical cancers, various types of applicators for HDR brachytherapy treatment are in use. The most common method for the ICBT treatment of cervical cancer is the Manchester system. The Manchester system-based ICBT approach is a more widely accepted method [5-9]. The Manchester system is characterized by doses to four points: Point A, Point B, bladder, and rectum. The duration of the implant is based on the dose rate at Point A, which is located 2 cm superior to the cervical os and 2 cm lateral to the cervical canal. Point B is defined as 3 cm laterally to Point A if the central canal is not displaced. If the tandem displaces the central canal, Point A moves with the canal, but Point B remains fixed at 5 cm from the midline.
In HDR brachytherapy, the applicator is first inserted into the patient, then the patient undergoes a CT-scan with the applicator inside and the same CT-scan is then transferred to the TPS. With the help of these computerized TPSs, the desired patient plan is created. In brachytherapy, the algorithm mostly used in TPS for dose calculations is based on the formalism presented by the American Association of Physicists in Medicine (AAPM) Task Group No. 43 Report (TG-43). The dose distribution in this report around brachytherapy sources is calculated using a variety of factors which are obtained through measurement or Monte Carlo simulation methods in a uniform phantom [10,11]. The TG-43 does not take heterogeneity correction within the human body into account and this formalism considers a bare source in the center of water for calculations [12-15]. However, in practice, various types of metallic central tandems and vaginal cylinders are used for the brachytherapy treatment of gynecological cancers [16] and TG-43 formalism effectively ignores the attenuation caused by metallic applicators and vaginal cylinders, which might lead to under dosage of the target while overestimating the dose to the OAR. So when the applicator geometry is not included in the TPS, there will be variation in the TPS calculated doses due to the different dosimetrical properties of these applicators [17].
The cervix applicator set studied in this study, consists of metallic central tandem of various angulations and vaginal cylinders of different diameters as shown in Fig. 1. These are Varian CT compatible applicators used in VariSource iX / VariSource 200/ GammaMed Plus iX / GammaMed Plus afterloader (Varian Medical Systems, Palo Alto, CA, USA) having Catalog number GM11004040. Although various types of applicators are in use for the brachytherapy treatment of cervical cancer, however, the attenuation in dose caused by this type of applicator and the applicator material has not been yet investigated. The attenuation of these applicators has been measured so that an accurate dose to the target and the organs at risk can be estimated when such applicators are used for cervical cancer treatment. In this study, the overestimation of dose by the BrachyVision TPS 11 (Varian Medical Systems) for these applicators was evaluated. The dose overestimation by TPS was obtained for tandem and cylinder assembly by using EBT3 Gafchromic films. Furthermore, a novel method, that is, well-type ionization chamber was used to find the attenuation due to various applicators used in gynecological brachytherapy, and the results obtained were compared with the results obtained by using Gafchromic films. In most of the other studies performed for such measurements, either only film dosimetry was done or a 0.125-mL ion chamber was used for dose measurements. The use of a 0.125-mL ion chamber for brachytherapy is cumbersome whereas the use of well-type ionization chamber for such measurements is relatively easy.
Materials and MethodsThis study has been carried out in the tertiary care hospital and the hospital is equipped with various state of art radiotherapy equipment. The HDR brachytherapy unit GammaMed Plus iX, has been used for this study. The GammaMed Plus iX is the 5th generation afterloader and has 24 channels. The GammaMed Plus iX afterloader and control software is designed to be fully compatible with hospital networks and enhance HDR and pulsed-dose rate (PDR) brachytherapy treatments. The HDR unit is fully integrated with the BrachyVision (version 11) TPS and the ARIA oncology information. The 192Ir radioactive source is housed in this GammaMed Plus iX afterloader HDR unit. The GammaMed Plus iX 192Ir HDR source consists of a 3.50-mm-long 192Ir core with a diameter of 0.70 mm, enclosed in a 0.90-mm-diameter and 4.52-mm-length AISI 316 L stainless steel capsule (density of 7.8 g/cm3) [18-20]. The 192Ir source emits a wide spectrum of relatively low energies, mostly in the range of 201–884 keV with an average value of 360 keV.
The unit is also provided with various applicators for brachytherapy treatment. The cervix applicators studied in this article include various vaginal cylinders and central metallic tandems. The vaginal cylinders are made up of polyetheretherketone (PEEK) having diameters of 20 mm, 23 mm, 26 mm, 30 mm, and 35 mm, and three types of stainless steel central metallic tandems having angulations of 0°, 20°, and 30° as shown in Fig. 1.
For the source strength verification of the GammMed Plus iX unit, HDR 1000 Plus well-type ionization chamber, and the electrometer with the appropriate source jig were used. The physical parameters of the HDR 1000 Plus well-type ionization chamber used in the hospital are given in Table 1 [21].
A total of 60 intracavitary brachytherapy insertions in 48 patients having a prescribed dose of 6 Gy at Point A, were studied for this article, four for each tandem and vaginal cylinder assembly. For the ICBT treatment of gynecological cancers, the appropriate metallic central tandem along with a vaginal cylinder was first inserted into the patient and then the patient had to undergo CT-scan. The CT data set was then transferred to the BrachyVision TPS. After segmentation of the target and OAR, i.e., bladder, rectum, and sigmoid, the reference points were defined (Reference Point A: left and right) and the dose of 6 Gy was prescribed at Point A [22] (Fig. 2). The dose optimization was done so that the OARs received the doses within the tolerance limit and the target receives the prescribed dose as per the standard guidelines. The plan, if found suitable was then approved by the radiation oncologist and then transferred to the control console wherein the various dwell positions with respective dwell times as programmed by the TPS are defined and the treatment was executed on the patient.
1. Measurement of dose using Gafchromic filmsThe approved patient treatment plan was delivered to a phantom mimicking patient set-up, with EBT3 Gafchromic film sheets, 1 cm × 1 cm in size, wrapped in thin, transparent polythene, and attached to the vaginal cylinder’s surface as shown in Fig. 3. The films were adhered with tape on the surface of the vaginal applicator in such a way that there was no air gap between the curved applicator surface and the films. The films were placed on the surface of the vaginal cylinder at known distances from the distal end of the vaginal cylinder so that the same area could be easily reproduced on the TPS. The tandem and vaginal cylinder assembly were then wrapped in elasto-gel bolus (water-based gels with acrylic polymer) of density 1.02 g/cm3 and thickness of 5 cm to simulate the backscatter within the patient.
For the accurate film dose measurements, the standard protocol was followed [23]. The EBT3 films were scanned using an EPSON scanner after initially being subjected to the known doses and the input data thus obtained was fed to OmniPro OmniPro software (IBA Dosimetry GmbH, Schwarzenbruck, Germany). The same EPSON scanner and OmniPro software were then used to measure the dose recorded on the exposed EBT3 films that were placed on the surface of vaginal cylinders.
2. Measurement of dose using well-type ionization chamberA well-type ionization chamber is often used in brachytherapy for dosimetric purposes. The well-type ionization chamber is provided with a unique source holder for each brachytherapy source and is commonly referred to as a source jig. To obtain the attenuation due to the various cervix applicators, the source jig was replaced with water equivalent elasto-gel to mimic the various vaginal cylinder sizes, as shown in Fig. 4. Now the measurements were made first with elasto-gel and then with the applicator assembly.
1) Case 1The plan which was created for the treatment of the patients was executed on HDR 1000 Plus well-type ionization chamber using elasto-gel of appropriate diameter as shown in Fig. 5A. The total charge collection by the electrometer was noted down.
2) Case 2In the second case, again the same plan was executed using HDR 1000 Plus a well-type ionization chamber but now instead of elasto-gel, the same tandem and vaginal cylinder assembly were used and the charge collection was measured as shown in Fig. 5B.
Pertinently in both the above cases, only the charge collection was measured and the calibration factor of the well-type chamber was not used in calculations which ensured that the calibration factor will not affect the final results obtained. It was also ensured in both the above cases that the distal end of the tandem and vaginal cylinder assembly and the distal end of the elasto-gel was placed at the same position in the base of the well-type ionization chamber and both were 12 cm deep within the well of the chamber. This ensured that the dwell positions of the 192Ir source in both the cases within the chamber were the same. Thus, in both cases, there was no difference in the comparative positions of the 192Ir source within the chamber.
A similar procedure was repeated for other patients wherein the patient was first inserted with appropriate tandem and vaginal cylinder assembly and then a plan was created on TPS and the same plan was executed with Gafchromic film taped on the surface of the applicator. Subsequently, the charge collection using a well-type ionization chamber was also measured. In this way, the results were obtained for all the different combinations of tandem and vaginal cylinder assembly.
The measured dose recorded by the Gafchromic films and the TPS calculated dose were compared using paired t-test, analyzed on the data editor of SPSS version 20 (IBM, Armonk, NY, USA). Also, the charge collected by well-type ionization chamber with elasto-gel and tandem-vaginal cylinder assembly was compared using the same test. A p-value less than 0.1 were considered significant.
ResultsThe dosimetric results were obtained both by using Gafchromic films and well-type ionization chamber. The mean overestimation of dose by the TPS was calculated for each tandem and vaginal cylinder assembly, using Gafchromic films. The results for 0°, 20°, and 30° angulated central tandems when used along with various diameters of vaginal cylinders are given in Tables 2–4, respectively. The mean percentage attenuation obtained by using a well-type ionization chamber due to 0°, 20°, and 30° central tandems when used along with various diameters of vaginal cylinders was also calculated and are given in Tables 5–7, respectively. Fig. 6 shows the mean overestimation of dose by the TPS for each tandem and vaginal cylinder assembly. The graphical representation of mean percentage attenuation for each tandem and vaginal cylinder assembly obtained by using a well-type ionization chamber is shown in Fig. 7.
It can be observed from the above tables that the maximum overestimation of dose by TPS is for 35-mm diameter vaginal cylinder when used along with 30º curvature central tandem and is 7.47% and is least for 0º central tandem when used with 20-mm vaginal cylinder and is 4.78%. The percentage attenuation values obtained by using well-type ionization chambers also showed that the maximum attenuation was by 35-mm diameter vaginal cylinder when used along with 30º curvature central tandem and is 6.82%, the least attenuation is for 0º central tandem when used with 20-mm vaginal cylinder and is 3.52%.
The results of the statistical analysis in both Gafchromic measurements and for well-type ionization chamber measurements showed that there is a significant decrease in dose when 30º angulated central tandem is used with a 35-mm vaginal cylinder (p < 0.10). However, for all other measurements, the difference was not significant (p > 0.10).
Discussion and ConclusionIn this study, the attenuation due to PEEK vaginal cylinders when used with stainless steel central tandems has been studied. The dosimetric influence of various vaginal cylinders, when used with different types of central tandems in brachytherapy, has been obtained using EBT3 Gafchromic films. In this study, a novel method that is the use of a well-type ionization chamber to find the attenuation due to various applicators used in brachytherapy was used and the results obtained were quite similar to the measurements using Gafchromic films.
The dose at the surface of the tandem and vaginal cylinder assembly was obtained by placing the Gafchromic films on the surface of the applicator. The dose recorded on the films was measured by using an Epson scanner with IMRT OmniPro software. The effect of tandem and vaginal cylinder assembly on net charge collection versus the charge collection with water equivalent elasto-gel was also studied using a well-type ionization chamber. The results obtained from these two methods gave effective attenuation due to tandem and vaginal cylinder assembly and the results in both the methods were analogous to each other with little variation.
The heterogeneity of the medium is not taken into account by the TPSs using the TG-43 algorithm for dose calculations. The TG-43 formalism effectively ignores the attenuation caused by vaginal cylinders and by metallic applicators, and thus the TPS calculated target, and OAR doses are overestimated and are presented in this study.
The percentage overestimation of dose by TPS for various tandem and vaginal cylinder assembly obtained in this study are shown in Tables 2–4. The percentage attenuation was also calculated for various tandems when used with different types of vaginal cylinders in well-type ionization chamber and it also showed almost the same trend with little respective variation and can be seen in Tables 5–7.
Sampath et al. [17] have studied the influence of central vaginal cylinders in HDR 192Ir brachy treatment with different diameter applicators. They have analyzed the dosimetric influence due to various vaginal cylinders of diameters 2.0, 2.5, 3.0, and 3.5 cm. They measured the dose by using a 0.125-mL ion chamber and the Oncentra planning system (Elekta, Stockholm, Sweden) was used for the dose calculation. The dose measured with the ion chamber was compared with EDR2 radiographic films. The authors conclude that the difference in TPS calculated and a measured dose is significant when high-density vaginal cylinders are used in measurement, which is consistent with our study. Parsai et al. [24] have studied the dose attenuation around Fletcher-Suit-Delclos due to stainless steel tube for HDR brachytherapy by using Monte Carlo calculations. The authors conclude that the patients may be receiving less dose due to metallic applicators. The authors further added that the anisotropy function has a predominant influence on dose reduction, whereas the radial dose function does not fluctuate too much as a result of attenuation. The authors suggested that the anisotropic and radial dose function of source in water used in treatment planning systems based on TG-43 formalism may be replaced with corresponding parameters of source applicator assembly.
In conclusion, this study is a step forward towards a better dose delivery in HDR ICBT treatment and evaluates the dose variation due to the brachytherapy TPS. The commercially available TPS used in brachytherapy calculates dose at various locations by using TG-43 formalism. To verify the TPS calculated doses, in vitro dose measurements of various tandems and vaginal cylinders by using EBT3 Gafchromic films were performed and the percentage attenuation due to various tandems and vaginal cylinders was also calculated by using a well-type ionization chamber.
The attenuation due to metallic central tandem and the vaginal cylinders used in brachytherapy treatment of gynecological cancers is more when compared to the attenuation due to water. Thus, the dose to the target as well as OAR is overestimated by the TPS in the HDR brachytherapy and should be taken into consideration while calculating the dose to the target and nearby organs at risk. The under dosage of the target if not considered may otherwise lead to treatment failures.
Fig. 1.The cervix applicator set including vaginal cylinders of diameters 35 mm, 30 mm, 26 mm, 23 mm, and 20 mm (from left to right) and central metallic tandems of angulations 0º, 20º, and 30º (from bottom to top). 
Fig. 2.Representative dose in color wash for 6 Gy prescription to Point A in multiplanar view and three-dimensional view. 
Fig. 3.(Top) Applicator surface taped with EBT3 Gafchromic films. (Bottom) Tandem and vaginal cylinder assembly wrapped in elasto-gel bolus. 
Fig. 4.Vaginal cylinders with respective diameter of water equivalent elasto-gel: (A) 35 mm, (B) 30 mm, (C) 26 mm, (D) 23 mm, and (E) 20 mm. 
Fig. 5.(A) Setup used to obtain charge collection when water equivalent elasto-gel. (B) Setup used to obtain charge collection when tandem and vaginal cylinder assemble was used. 
Fig. 6.Mean percentage overestimation of dose by treatment planning system (TPS) for various tandem-vaginal cylinder assembly. 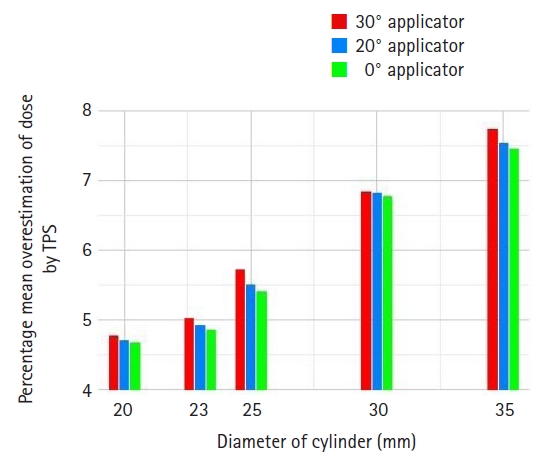
Fig. 7.Mean percentage attenuation by various tandem and vaginal cylinder assembly obtained by using well-type ionization chamber. 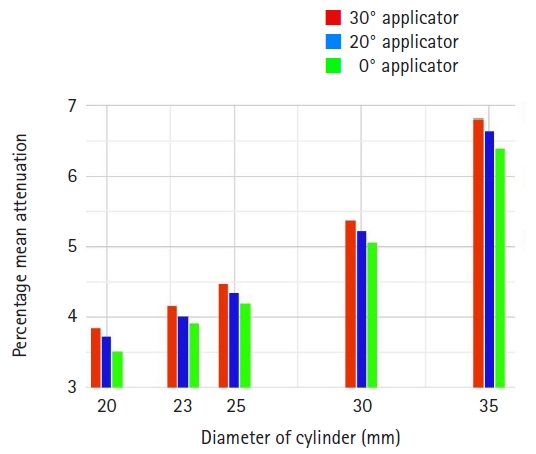
Table 1.Physical parameters of HDR 1000 Plus well-type ionization chamber
Table 2.Comparison of mean in vivo doses and calculated (TPS) doses in ICBT with 0º central tandem and vaginal cylinder assembly
Table 3.Comparison of mean in vivo doses and calculated (TPS) doses in ICBT with 20º central tandem and vaginal cylinder assembly
Table 4.Comparison of mean in vivo doses and calculated (TPS) doses in ICBT with 30º central tandem and vaginal cylinder assembly
Table 5.Mean attenuation due to 0º central tandem when used with various vaginal cylinders Table 6.Mean attenuation due to 20º central tandem when used with various vaginal cylinders Table 7.Mean attenuation due to 30º central tandem when used with various vaginal cylinders References1. Sankaranarayanan R, Ferlay J. Worldwide burden of gynaecological cancer: the size of the problem. Best Pract Res Clin Obstet Gynaecol 2006;20:207–25.
2. Yi M, Li T, Niu M, Luo S, Chu Q, Wu K. Epidemiological trends of women’s cancers from 1990 to 2019 at the global, regional, and national levels: a population-based study. Biomark Res 2021;9:55.
3. Rose PG, Bundy BN, Watkins EB, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med 1999;340:1144–53.
4. Tyree WC, Cardenes H, Randall M, Papiez L. High-dose-rate brachytherapy for vaginal cancer: learning from treatment complications. Int J Gynecol Cancer 2002;12:27–31.
5. Roy S, Subramani V, Singh K, Rathi AK, Savita A, Aditi A. Study of the effects of dwell time deviation constraints on inverse planning simulated annealing optimized plans of intracavitary brachytherapy of cancer cervix. J Cancer Res Ther 2019;15:1370–6.
6. Fellner C, Pötter R, Knocke TH, Wambersie A. Comparison of radiography- and computed tomography-based treatment planning in cervix cancer in brachytherapy with specific attention to some quality assurance aspects. Radiother Oncol 2001;58:53–62.
7. Schoeppel SL, LaVigne ML, Martel MK, McShan DL, Fraass BA, Roberts JA. Three-dimensional treatment planning of intracavitary gynecologic implants: analysis of ten cases and implications for dose specification. Int J Radiat Oncol Biol Phys 1994;28:277–83.
8. Kapp KS, Stuecklschweiger GF, Kapp DS, Hackl AG. Dosimetry of intracavitary placements for uterine and cervical carcinoma: results of orthogonal film, TLD, and CT-assisted techniques. Radiother Oncol 1992;24:137–46.
9. Ling CC, Schell MC, Working KR, et al. CT-assisted assessment of bladder and rectum dose in gynecological implants. Int J Radiat Oncol Biol Phys 1987;13:1577–82.
10. Williamson JF, Li Z. Monte Carlo aided dosimetry of the microselectron pulsed and high dose-rate 192Ir sources. Med Phys 1995;22:809–19.
11. Rivard MJ, Butler WM, DeWerd LA, et al. Supplement to the 2004 update of the AAPM Task Group No. 43 report. Med Phys 2007;34:2187–205.
12. Nath R, Anderson LL, Luxton G, Weaver KA, Williamson JF, Meigooni AS. Dosimetry of interstitial brachytherapy sources: recommendations of the AAPM Radiation Therapy Committee Task Group No. 43. Med Phys 1995;22:209–34.
13. Rivard MJ, Coursey BM, DeWerd LA, et al. Update of AAPM Task Group No. 43 report: a revised AAPM protocol for brachytherapy dose calculations. Med Phys 2004;31:633–74.
14. Sampath G, Anbazhagan S, Lokhande CD. Analysis of central vaginal cuff HDR brachytherapy using various cylinder sizes-literature review. Oncol Radiother 2021;15:1–4.
15. Mozaffari A, Ghorbani M. Determination of TG-43 dosimetric parameters for photon emitting brachytherapy sources. J Biomed Phys Eng 2019;9:425–36.
16. Gadda IR, Khan NA, Wani SQ, Baba MH. To evaluate the use of tandem and cylinder as an intracavitary brachytherapy device for carcinoma of the cervix with regard to local control and toxicities. J Cancer Res Ther 2022;18:740–6.
17. Sampath G, Anbazhagan S, Lokhande CD. The dosimetric influence of central vaginal cylinders in high dose rate (HDR) iridium (Ir192) brachytherapy treatment. J Chalmeda Anand Rao Inst Med Sci 2019;17:7.
18. Taylor RE, Rogers DW. EGSnrc Monte Carlo calculated dosimetry parameters for 192Ir and 169Yb brachytherapy sources. Med Phys 2008;35:4933–44.
19. Ballester F, Puchades V, Lluch JL, et al. Technical note: Monte-Carlo dosimetry of the HDR 12i and Plus 192Ir sources. Med Phys 2001;28:2586–91.
20. Perez-Calatayud J, Ballester F, Das RK, et al. Dose calculation for photon-emitting brachytherapy sources with average energy higher than 50 keV: report of the AAPM and ESTRO. Med Phys 2012;39:2904–29.
21. Vandana S, Sharma SD. Long term response stability of a well-type ionization chamber used in calibration of high dose rate brachytherapy sources. J Med Phys 2010;35:100–3.
22. Nag S, Erickson B, Thomadsen B, Orton C, Demanes JD, Petereit D. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys 2000;48:201–11.
23. Gafchromic EBT3 specifications [Internet]. Bridgewater, NJ: Ashland Advanced Materials; c2022 [cited 2022 Sep 1]. Available from: http://www.gafchromic.com/documents/EBT3_Specifications.pdf.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |