Low body mass index is associated with poor treatment outcome following radiotherapy in esophageal squamous cell carcinoma
Article information
Abstract
Purpose
We aimed to determine whether patients with esophageal cancer with a low baseline body mass index (BMI) have a poor prognosis following radiotherapy (RT).
Materials and Methods
We retrospectively analyzed data from 50 patients with esophageal cancer to determine whether a low starting BMI (before RT) was associated with a poor outcome. All study participants were diagnosed with non-metastatic esophageal squamous cell carcinoma (SCC).
Results
The number of patients at each T stage were as follows: 7 (14%) patients at T1, 18 (36%) at T2, 19 (38%) at T3, and 6 (12%) at T4. Based on BMI, 7 (14%) patients were defined as underweight. A low BMI was common in patients with T3/T4 stage esophageal cancer (7/43, p = 0.01). Overall, the 3-year progression-free survival (PFS) and overall survival (OS) rates were 26.3% and 69.2%, respectively. In univariate analysis, clinical factors associated with poor PFS included being underweight (BMI <18.5 kg/m2; p = 0.011) and a positive N status (p = 0.017). Univariate analysis also revealed that being underweight was associated with a decrease in OS (p = 0.003). However, being underweight was not an independent prognostic factor for PFS and OS.
Conclusion
Patients with esophageal SCC with a low starting BMI (BMI <18.5 kg/m2) are more prone to have a negative survival outcome following RT than patients who are considered to be normal weight or overweight. For this reason, it is important that clinicians pay more attention to BMI when treating patients with esophageal SCC.
Introduction
Weight loss has been extensively studied as a prognosis for treatment outcome in patients with cancer [1,2]. Pretreatment-associated weight loss has been shown to be detrimental for patients with cancer, and the prognosis is poor for cancers in specific gastrointestinal sites, including the stomach, pancreas, and esophagus [2]. Moreover, several reports have shown an association of body mass index (BMI) with both the incidence and prognosis of esophageal cancer [3,4]. Furthermore, a low BMI (i.e., <18.5 kg/m2) is a risk factor for mortality in patients with esophageal squamous cell carcinoma (SCC). For example, in 2007, Smith et al. [5] reported that patients with a high BMI had a lower mortality rate than patients with a normal or low BMI. A recent study by Gu et al. [6] also reported that patients with higher BMI exhibited longer survival. According to a recent study by Liu et al. [7], weight loss and high TNM stage were adverse prognostic factors for patients with esophageal SCC. In addition, based on a recent large-scale study in China by Ren et al. [4], underweight patients tended not to receive adjuvant chemotherapy, and high BMI was associated with better disease-specific survival. Finally, case control study in Australia by Lahmann et al. [8] also showed that high BMI was associated with a low risk of esophageal SCC regardless of smoking status. In contrast, Loehrer et al. [9] found that obese patients with adenocarcinoma had a worse prognosis compared to patients with normal BMI. Furthermore, Blom et al. [10] reported that the effect of BMI on prognosis was no longer apparent in patients with esophageal cancer who underwent esophagectomy. However, Chen et al. [11] reported that disease-free survival was shorter in patients with a high BMI who underwent surgery than in patients with a low to normal BMI.
In this study, we sought to evaluate whether baseline BMI is associated with treatment outcome in patients with esophageal SCC receiving curative RT. We also assessed the relationship between BMI and other clinical factors, such as T stage, N stage, and underlying type 2 diabetes. In addition, we analyzed the relationship between RT interruption and BMI. In 2013, 96% of reported esophageal cancers in Korea were SCC [12]. Therefore, study results reflect outcomes of radiotherapy (RT) in Korean patients with esophageal cancer.
Materials and Methods
1. Patient population
We retrospectively analyzed data from 50 patients with esophageal cancer who underwent curative RT as a first-line treatment. The study was conducted at Inje University Busan Paik Hospital, from December 2009 to January 2022. All patients were pathologically diagnosed with esophageal SCC before RT was initiated. None of the patients included in this study had stent insertion or feeding gastrostomy before RT. This study was approved by the Institutional Review Board in Busan Paik Hospital (IRB No. 2022-03-035). The informed consent was waived.
BMI was calculated according to the patient’s medical records by dividing their weight in kilograms by their height in meters squared. Patients were defined as underweight, normal weight, and overweight based on a BMI of <18.5 kg/m2, 18.5–24.9 kg/m2, and >25 kg/m2, respectively.
Patients were grouped as ever or never smokers. Alcohol abuse was categorized by obtaining a social history for each patient. Data on patient medical history about metabolic syndrome, such as diabetes and hyperlipidemia, was collected.
Tumor location was defined as occurring at three levels: upper thoracic esophagus (20–25 cm from the upper incisors), middle thoracic esophagus (25–30 cm from the upper incisors), and lower thoracic esophagus (30–50 cm from the upper incisors).
Our hypothesis in this study was that a lower body weight would be associated with poor treatment outcome following RT in patients with esophageal SCC. A relationship between BMI and the prognosis of patients with esophageal SCC has been previously shown in a study by Skipworth et al. [13] in 2009. According to a recent study by Liu et al. [7], weight loss and high TNM stage were adverse prognostic factors in patients with esophageal SCC. In addition, according to a recent large scale study in China by Ren et al. [4], underweight patients tended not to receive adjuvant chemotherapy, and high BMI was associated with better disease-specific survival. Therefore, in this study, we evaluated the prognostic effects of BMI in patients with esophageal SCC.
Arc intensity-modulated RT was planned for treatment. For radiation fields, the target volume was established as a 3–5 cm margin superiorly and inferiorly and as a 1-cm margin laterally in each direction relative to the primary tumor. Positron emission tomography with integrated computed tomography was used for contouring the tumor volume. RT was usually administered at a total dose of 50.4 Gy. A daily dose of 1.8–2 Gy per fraction was administered. RapidArc and VitalBeam (Varian Medical System, Palo Alto, CA, USA) were used for external beam RT.
Most patients received concurrent chemoradiotherapy. The common chemotherapy regimen during RT was several cycles of 5-fluorouracil and cisplatin (FP).
The primary outcome was progression-free survival (PFS), which was defined as the length of time between the initial diagnosis and either recurrence or the last follow-up (death was not included). The secondary outcome was overall survival (OS). PFS and OS were calculated from the date of pathologic diagnosis to the date of each event.
2. Inclusion and exclusion criteria
Patients included in this study were all older than 18 years of age. Patients diagnosed with distant metastases during their initial treatment were excluded from the study. Patients treated with less than 40 Gy for the cumulative dose for RT were also excluded, as this was considered as an insufficient radiation dose for curative therapy.
3. Statistical methods
The chi-squared test was used to determine clinical factors associated with disease progression. Significance was set at p < 0.05. Fisher exact test was used in this study. The Kaplan–Meier test was used to estimate PFS and OS, and the log-rank test was used to find factors related survival. In addition, the Cox regression proportional hazards model was used to define independent prognostic factors that were related to survival. MedCalc statistical software (MedCalc Software, Mariakerke, Belgium) and SPSS version 24 (IBM, Armonk, NY, USA) was used for statistical evaluation.
Results
1. Patient characteristics and treatment
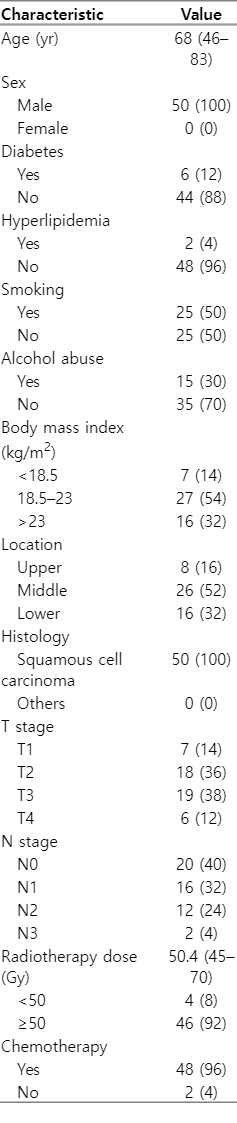
The median follow-up period of the study was 9 months. Patient characteristics are outlined in Table 1.
The patients enrolled this study were all older than 40 years of age (median, 68 years; range, 46 to 83 years). All patients had SCC. The number of patients at each T stage were as follows: 7 (14%) patients at T1, 18 (36%) at T2, 19 (38%) at T3, and 6 (12%) at T4. In addition, 30 (60%) patients had nodal metastases at diagnosis. Based on BMI, 7 (14%), 27 (54%), and 16 (32%) patients were defined as underweight, normal weight, and overweight, respectively. A total of six patients (12%) had type 2 diabetes. In addition, two patients (4%) had hyperlipidemia. Half of patients (n = 25; 50%) were smoker, and 15 patients (30%) were categorized as alcohol abuse.
Most patients (96%) received chemotherapy concurrently with RT. The most common chemotherapy regimen (n = 40; 80%) during RT was two or three cycles of FP every 3 weeks. Cisplatin chemotherapy alone every 3 weeks was used in 8 (16%) patients. The remaining two patients only received RT. Regarding the total radiation dose, the majority of patients (n = 46; 92%) received ≥50 Gy.
2. Progression pattern
During the median 9-month follow-up period (range, 1.5 to 85.7 months), 29 patients experienced disease progression. The disease progression rate did not differ based on prognostic factors (Table 2). Underweight did not significantly increase the incidence of failure (p = 0.635) (Table 2). More specifically, 21 (42%) patients experienced locoregional failure, and 11 (22%) patients showed distant failure. Among the patients with distant failure, three also experienced locoregional failure. Moreover, 19.0% (4/21) of patients who experienced locoregional failure were underweight.
3. Survival analysis
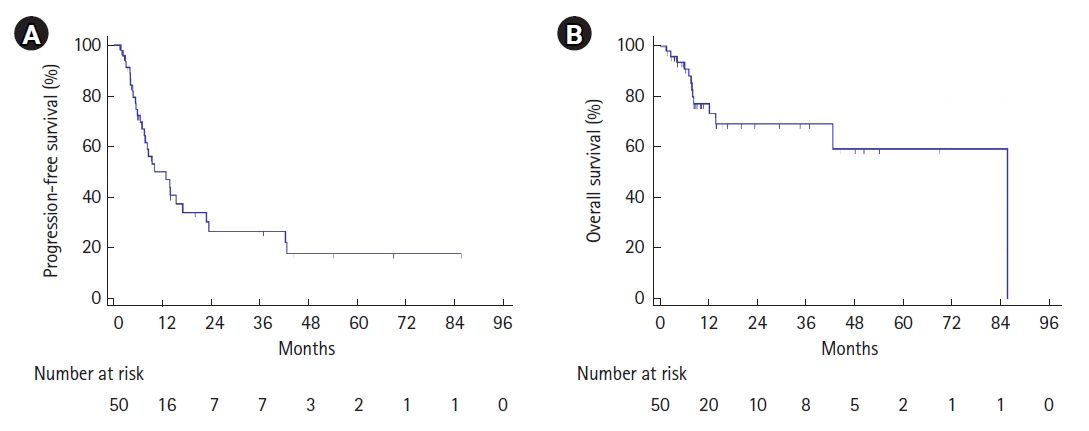
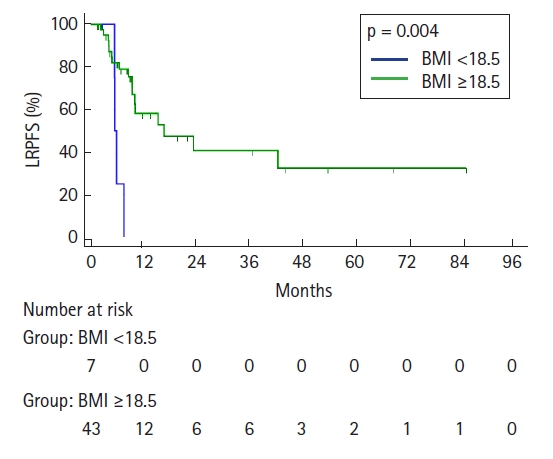
Overall, the 3-year PFS and OS rates were 26.3% and 69.2%, respectively (Fig. 1A, 1B). The 3-year locoregional PFS rate (LRPFS) was 36.6%.
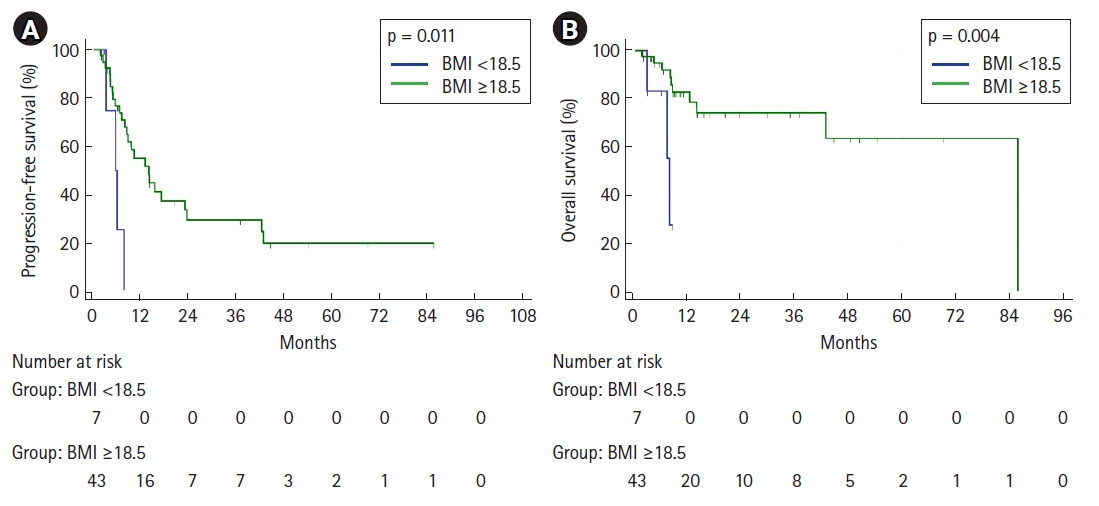
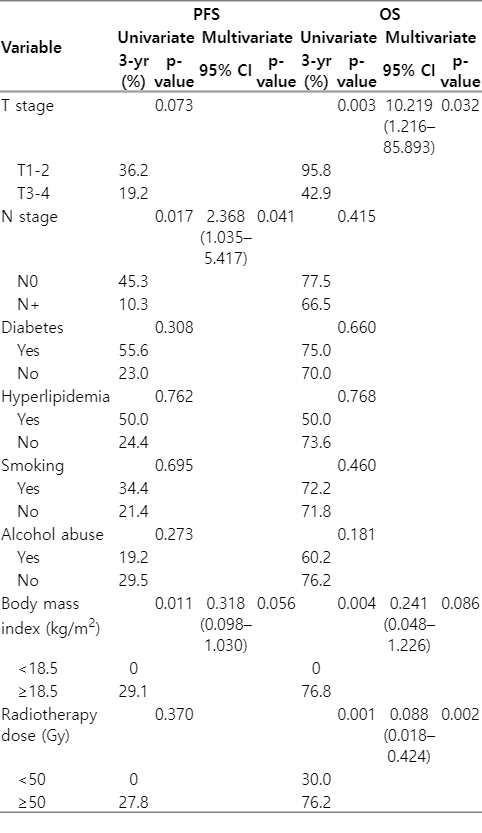
Table 2 shows the prognostic factors related OS and PFS. Univariate analysis revealed that both N stage and being underweight were associated with a lower PFS (p = 0.017 and p = 0.011, respectively) (Fig. 2A). Advanced T stage (T3/T4) tended to be negatively associated with PFS (p = 0.073) (Table 3). However, smoking and alcohol abuse did not reduce the PFS and OS (Table 3). Being underweight (p = 0.004) (Fig. 2B) and receiving a total radiation dose <50 Gy (p = 0.001) (Table 2) was associated with a low OS.
We also found that being underweight was associated with impaired locoregional progression and significantly associated with a low LRPFS (p = 0.004) (Fig. 3). Except for underweight, there were no other prognostic factors associated with LRPFS in the univariate analysis.
Multivariate analysis showed that N stage was an independent prognostic factor for PFS and that total radiation dose was an independent prognostic factor for OS (Table 3). However, being underweight was not an independent prognostic factor for PFS or OS.
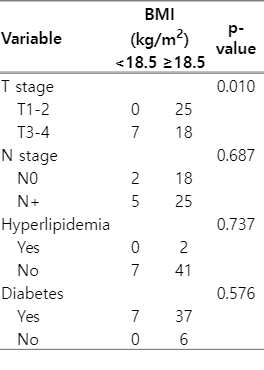
4. Correlation between body mass index and clinical factors
Table 4 shows the correlation between advanced T stage (T3/T4) disease and being underweight. A low BMI was common in patients with T3/4 stage esophageal cancer (7/43, p = 0.010) (Table 4). Neither positive N stage nor diabetes was associated with low BMI.
5. Treatment interruption
Treatment interruption during RT (total RT period >50 days) occurred in 11 patients, and it occurred more frequently in underweight patients compared to that in normal or overweight patients (4/7 vs. 7/43, p = 0.034). However, treatment interruption during RT was not statistically related with increased disease progression rates (p = 0.741).
Discussion and Conclusion
The present results suggest that a patient's pre-treatment weight greatly influences treatment outcome following RT in esophageal SCC. Furthermore, advanced T stage (T3/T4) was correlated with pre-treatment low body weight in esophageal SCC. This study provides useful clinical information for the management of patients with esophageal cancer.
These results confirm that a low body weight is a poor prognosis for patients with esophageal SCC. Zhang et al. [14] reported similar findings that pre-treatment low body weight was associated with poor treatment outcome in patients with esophageal cancer. However, the authors [14] recognized that other factors besides weight loss, such as stage, may have indirectly affected these poor treatment outcomes. Moreover, a case control study in Australia by Lahmann et al. [8] also showed that high BMI was associated with a low risk of esophageal SCC regardless of smoking status. Furthermore, according to a study by Button et al. [15], SCC usually has a longer lesion length compared to that of adenocarcinoma and frequently exhibits esophageal wall narrowing [8], which is more correlated with weight loss. Severe weight loss weakens the immune system and can easily exacerbate esophageal cancer. The current results also demonstrate that advanced T stage was associated with a low body weight before RT. Moreover, RT interruption occurred more frequently in patients with low BMI, i.e., underweight patients who did not receive a full dose of RT were more likely to suffer complications related to lowered immunity, such as leukopenia.
Similarly, sarcopenia seems to influence the survival outcomes for esophageal cancer patients treated with neoadjuvant chemoradiotherapy. According to a recent study by Yoon et al. [16], excessive muscle loss (skeletal muscle index <-10.0% in 50 days) was significantly associated with OS. Furthermore, Reisinger et al. [17] also argued that muscle mass loss during neoadjuvant chemoradiotherapy was related to postoperative mortality in patients with advanced stage esophageal cancer.
To avoid detrimental treatment outcomes because of weight loss or low pre-treatment weight, nutritional support should be provided to patients with esophageal cancer. Indeed, a study by Davies et al. [18] reported that early nutritional support and intervention may be helpful in improving the overall condition of patients with esophageal cancer, as an increase in mortality has been noted in patients with severe weight loss (i.e., >10% of starting weight).
Stent insertion or feeding gastrostomy [19] may aid in improving a patients’ nutritional condition. Whether stent insertion improves the overall health of patients remains debatable, but it would appear that providing patients with supplemental nutrition is a good option [20,21]. Additionally, post-RT stenting may aid in condition recovery in patients with esophageal cancer. Iwagami et al. [20] reported that esophageal metal stent insertion before RT contributed to a reduction in severe adverse events. Ogino and Akiho [19] also noted that percutaneous feeding gastrostomy could be useful for nutritional support in esophageal cancer. Considering the above, further studies are required to determine whether alleviation of dysphagia by medical devices, such as stent insertion or feeding gastrostomy, improves the patient’s overall medical condition and nutritional status [18].
We acknowledge several limitations in our study. Firstly, the number of enrolled patients was limited due to the single, retrospective study design. Secondly, the weight of the patients was not continuously monitored throughout the study, and body weight was only recorded before the commencement of RT. Thirdly, BMI was not an independent prognostic factor of survival in multivariate analysis, even though low BMI was significantly clinical factor for PFS and OS in univariate analysis. BMI may be not independent factor because of small sample size. Further analysis revealed that advanced T stage disease influenced BMI.
In conclusion, a low starting BMI tends to be an adverse clinical factor for survival outcome in patients with esophageal SCC undergoing curative RT, even though it is not independent factor. Patients that were underweight at diagnosis commonly manifested advanced T stage disease. These results suggest that clinicians should pay special attention to underweight patients with esophageal cancer. Further studies investigating the effect of active nutritional support in underweight patients with esophageal SCC during and after RT are required to improve treatment outcome in these patients.
Notes
Statement of Ethics
This study was approved by the Institutional Review Board in Busan Paik Hospital (IRB No. 2022-03-035).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author Contributions
Conceptualization, YC, JL. Investigation and methodology, YC, JL. Writing of the original draft, YC. Writing of the review and editing, JL, YC. Formal analysis, YC.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.