Proton therapy for reducing heart and cardiac substructure doses in Indian breast cancer patients
Article information
Abstract
Purpose
Indians have a higher incidence of cardiovascular diseases, often at a younger age, than other ethnic groups. This higher baseline risk requires consideration when assessing additional cardiac morbidity of breast cancer treatment. Superior cardiac sparing is a critical dosimetric advantage of proton therapy in breast cancer radiotherapy. We report here the heart and cardiac-substructure doses and early toxicities in breast cancer patients treated post-operatively with proton therapy in India’s first proton therapy center.
Materials and Methods
We treated twenty breast cancer patients with intensity-modulated proton therapy (IMPT) from October 2019 to September 2022, eleven after breast conservation, nine following mastectomy, and appropriate systemic therapy, when indicated. The most prescribed dose was 40 GyE to the whole breast/chest wall and 48 GyE by simultaneous integrated boost to the tumor bed and 37.5 GyE to appropriate nodal volumes, delivered in 15 fractions.
Results
Adequate coverage was achieved for clinical target volume (breast/chest wall), i.e., CTV40, and regional nodes, with 99% of the targets receiving 95% of the prescribed dose (V95% > 99%). The mean heart dose was 0.78 GyE and 0.87 GyE for all and left breast cancer patients, respectively. The mean left anterior descending artery (LAD) dose, LAD D0.02cc, and left ventricle dose were 2.76, 6.46, and 0.2 GyE, respectively. Mean ipsilateral lung dose, V20Gy, V5Gy, and contralateral breast dose (Dmean) were 6.87 GyE, 14.6%, 36.4%, and 0.38 GyE, respectively.
Conclusion
The dose to heart and cardiac substructures is lower with IMPT than published photon therapy data. Despite the limited access to proton therapy at present, given the higher cardiovascular risk and coronary artery disease prevalence in India, the cardiac sparing achieved using this technique merits consideration for wider adoption in breast cancer treatment.
Introduction
Cardiovascular disease has an earlier onset and a more lethal course in Indians and other South Asians than in other population groups; this propensity has been noted to persist even in the diaspora [1]. In addition, a significant number of Indians suffer from diabetes and hypertension, both of which increase the propensity for cardiovascular ailments [2].
Even as the incidence of breast cancer rises [3], mortality due to the disease has declined [4]. A recently published audit of more than 2,000 breast cancer patients treated in a single year, at one of India’s largest cancer centres, documented a 5-year disease-free survival of 85% for early and 68% for locally advanced breast cancer patients, respectively [5]. This makes the issues of survivorship relevant; one of these is treatment-related cardiac side-effects [4].
Cardiac ailments account for the highest number of non-cancer deaths in breast cancer patients. Deaths from cardiac causes constitute 10.1% of all deaths within one year and 19%, i.e., nearly a fifth of all deaths in patients surviving >10 years after breast cancer diagnosis [6].
Several systemic treatments, such as adriamycin, taxanes, trastuzumab, and letrozole are cardiotoxic [7-10]. Though the cardiotoxicity of radiotherapy has declined due to the development of better techniques [11] it remains relevant, with dose-volume parameters being better understood now.
Darby et al. [12] defined acute coronary events (ACEs) as the diagnosis of myocardial infarction, coronary revascularization, or death resulting from ischemic heart disease after completion of treatment. The authors noted a 7.4% increase in the relative risk of an ACE for every 1 Gy increase in mean heart dose with no lower threshold of radiation dose for these events. Prior ischemic heart disease (IHD) markedly increased the odds of an ACE 6.67 times; hypertension, diabetes, chronic obstructive pulmonary disease (COPD), obesity and smoking also nearly doubled the risk, even with no history of IHD.
Subsequent to Darby’s landmark study [12], there has been a further analysis on the dose-volume relationship of cardiac toxicity and the dose received by cardiac substructures; coronary arteries and the left ventricle have emerged as organs-at-risk (OARs) [13,14]. In a prospective study by Abraham et al. [14], 17% of left-sided breast cancer patients, with only a small fraction receiving adriamycin and trastuzumab, had some form of cardiac ailment.
A review of mean heart doses published after 2014 has noted a mean heart dose of 3.6 Gy for left-sided breast cancer patients and 4.8 Gy in left-sided patients receiving a boost with photon therapy [15]. In contrast, mean heart doses in both dosimetric and clinical studies of proton therapy for breast cancer, are <1.5 Gy and <1 Gy for left and right-sided lesions, respectively [16]. Proton therapy, delivered by enface beams, is an elegant method to treat the breast/chest wall while reducing the dose to the heart and cardiac substructures [17,18]. Mutter et al. [19] have published a consensus statement that comprehensively discusses the role, technique & impact of proton therapy across various clinical scenarios.
Proton therapy has recently become available in India. A prospective registry HYPRO-B has been initiated to document the impact of proton therapy in Indian breast cancer patients. We report the dosimetric and early clinical outcomes of 20 consecutive breast cancer patients treated using pencil beam-based proton therapy in the region’s first proton therapy center.
Materials and Methods
Proton therapy was initiated in January 2019 and the first breast patient was treated in October 2019. We reviewed the details of 20 consecutive patients treated for breast cancer with proton therapy. The latter 16 patients were included in the HYPRO-B registry (HYpofractionated PROton therapy in Breast cancer). This study was approved by the Institutional Ethics Committee-Biomedical Research, Apollo Hospitals, Chennai, India (IEC No. API-I-C-S-004110-20). All patients were treated after informed consent.
1. Proton therapy planning and delivery protocol
Patients were immobilized in the supine position, with arms above the head on a breast board (Access Supine Breast Device, Avondale, PA, USA), and a planning CT was performed with axial images of 2 mm thickness on Canon Aquilion LB CT scanner.
The clinical target volume (CTV) structures, including whole breast/chest wall and nodal volumes, were contoured as per the RTOG atlas [20]; these were clipped 5mm (for the whole breast) and 3 mm (for chest wall) from the skin, respectively. In one patient the chest wall volume was not clipped, because of the involvement of dermal lymphatics. The supraclavicular lymph node region extended to the midline medially, the cricoid superiorly, trapezius posteriorly and followed the medial edge of the clavicle laterally. OARs, including the heart, left lung, right lung, esophagus, and thyroid, were contoured. Fifteen cardiac segments (five left ventricular and 10 coronary arterial segments) were delineated as per the cardiac contouring atlas described by Duane et al. [21]. A 3-5 mm rib rind was contoured outward from the rib pleural interface to encompass the rib cage.
Proton therapy treatment was planned on a RayStation treatment planning system (version 9.0; RaySearch Laboratories AB, Stockholm, Sweden). The dose prescription was 40 GyE to whole breast/chest wall, 48 GyE simultaneous integrated boost (SIB) to tumour bed and 37.5 GyE to nodal volumes, supraclavicular region, axilla & internal mammary chain (IMC) in 20 fractions. The first four patients were treated with a more protracted 20-fraction regime. Standard fractionation of 50 Gy in 2 Gy per fraction was advised to patients with a rheumatoid disorder or a silicone implant in situ. Two en-face beams were used with a hinge angle of 20°–30° (Fig. 1). A water-equivalent 4 cm Lucite range shifter was used for each beam. The CTV was robustly optimized for a 3-mm setup and 3.5% range uncertainty. Both dose computation and optimization used a Monte Carlo algorithm. An average relative biological equivalent (RBE) of 1.1 was used and all patients were planned with single-field optimization (SFO) technique. The planning goal considered was ideal target coverage of CTV, i.e., 97% of the target to receive at least >95% of the prescribed dose.
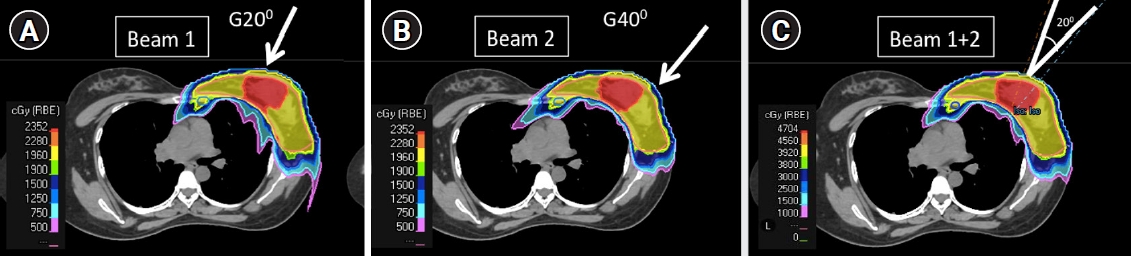
Axial slice from treatment plan showing two en-face beam arrangements for a left sided breast patient (whole breast + tumor bed [SIB]). (A) Beam 1 is gantry at 20°, (B) Beam 2 is gantry at 40°, and (C) isodose distribution after a combination of two beams.
Treatment was delivered using pencil beam scanning protons on Proteus Plus machine (IBA, Louvain-La-Neuve, Belgium), where in each energy layer is scanned (from –X to +X direction of every Y coordinate) as seen in the beam’s eye view (BEV) of particular beam geometry. For proton energies between 70.22 and 226.2 MeV, the in-air X (Y) spot sigma at the isocenter ranges from 2.96 (3.00) to 6.68 (6.52) mm.
Treatment was delivered 5 times a week, with daily CBCT based image guided repositioning and intra-treatment monitoring using AlignRT (version 5.1.2; VisionRT, London, UK) based surface guidance. AlignRT is integrated with beam delivery system of Proteus Plus using universal beam triggering interface (UBTI). It allows pausing of the beam when the breathing amplitude of the patient exceeds the set threshold (±3 mm).
2. Outcome assessment
1) Dosimetric
Coverage and OAR doses were documented as per dose prescription. Proton therapy plans were assessed for coverage of CTV 40 Gy, 37.5 Gy, 48 Gy by 95% of prescription dose, mean heart dose, mean and D0.02cc of left anterior descending artery (LAD) and right coronary artery (RCA), Dmax oesophagus, Dmax spinal cord, mean lung dose, mean ipsilateral and contralateral lung dose, V20Gy and V5Gy ipsilateral and contralateral lung and mean contralateral breast dose.
2) Clinical
All patients were reviewed weekly once during radiation therapy, 4 weeks after therapy and then at 3 monthly intervals.
Results
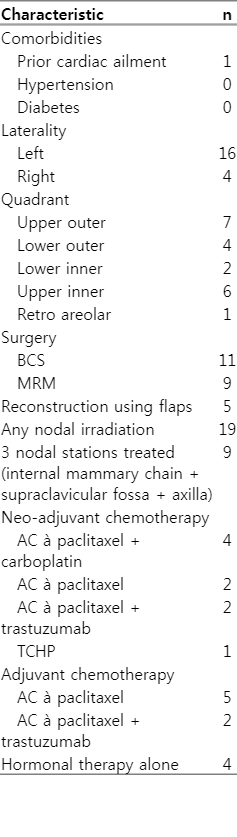
Eleven patients received proton therapy following breast-conserving surgery (BCS), one after a skin-sparing mastectomy and the remaining received radiation following a mastectomy (Table 1). One patient did not require regional nodal irradiation. Among the 19 patients requiring nodal irradiation, nine received composite irradiation to three nodal regions; axillary radiation was omitted in the remaining 11 patients. All patients undergoing proton therapy after BCS received a boost to the tumour bed.
Adjuvant/neoadjuvant systemic treatment included adriamycin in 13, taxanes in 16, and trastuzumab in five. The remaining patients received hormone therapy alone.
Cardiovascular risk factors were present in six patients, diabetes in two, hypertension in three, rheumatoid arthritis in two, obesity in one and previous heart ailment in one patient, respectively; four patients had multiple risk factors (>1).
1. Target
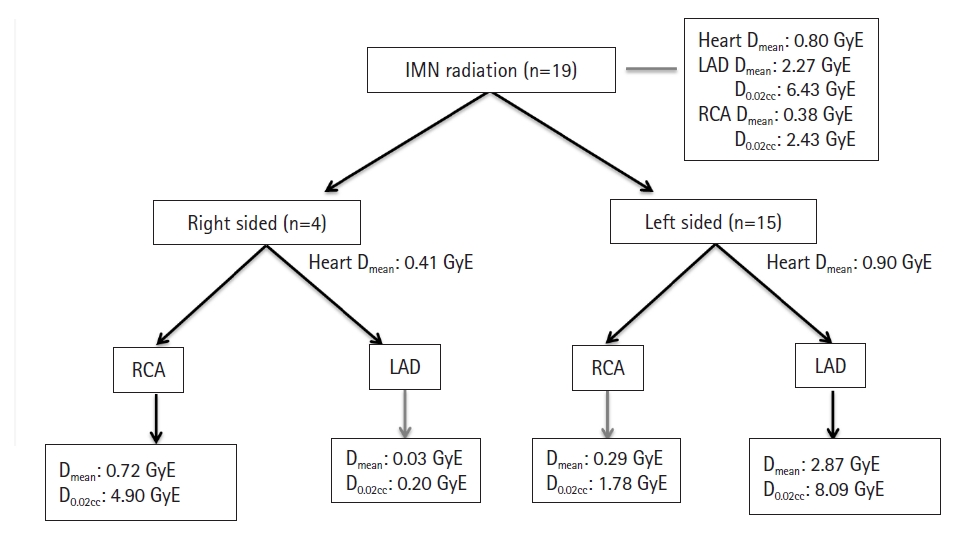
Proton therapy achieved adequate dose coverage of breast/chest wall, i.e., CTV40, with a mean 99% of the target receiving 95% of the prescribed dose (V95% > 99%). Similarly, 99% of the regional nodes (internal mammary, supraclavicular, and axilla) atleast 95% of the prescribed dose. The OAR doses and V95% of the target are shown in Fig. 2 and Tables 2, 3. The dosimetric outcomes of patients had internal mammary nodal irradiation are shown in Fig. 3.
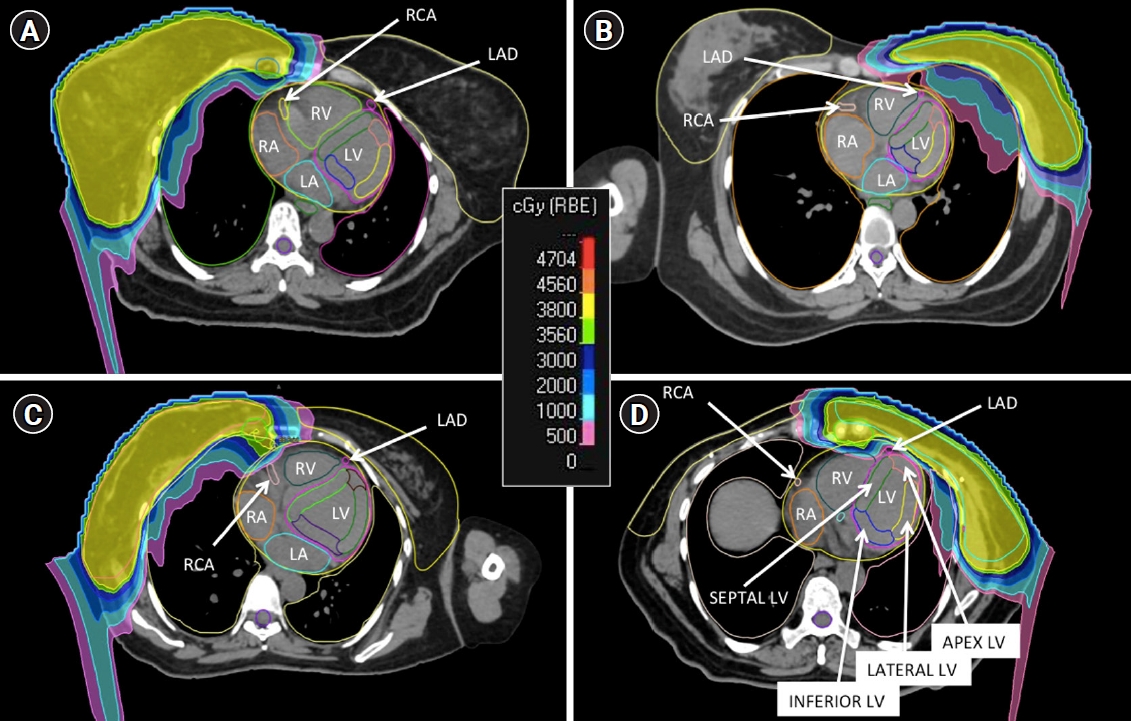
Radiation dose color wash of (A) right breast post-BCS, (B) left breast post-BCS, (C) right chest wall (with reconstruction), and (D) left chest wall, at the level of the left ventricle, showing coronary arterial segments and left ventricular myocardial segments. BCS, breast conservation surgery; RCA, right coronary artery; LAD, left anterior descending artery; RA, right atrium; RV, right ventricle; LA, left atrium; LV, left ventricle.
2. OAR
The mean heart dose was 0.78 GyE, 0.41 GyE in patients with right-sided cancer and 0.88 GyE in patients with left-sided cancer. Among left-sided patients, the mean heart dose was 0.991 GyE for patients receiving chest wall proton therapy and 0.79 GyE for patients being irradiated following BCS; this was 0.475 GyE and 0.345 GyE, respectively, for right-sided patients. The mean ipsilateral lung dose was 6.84 GyE, V17 of 14.6%, and V4 of 36.4%.
3. Cardiac substructures
The mean LAD dose of the cohort was 2.76 GyE. The high-dose region likely to correlate with the location of coronary stenosis was analyzed as the minimum dose received by 0.02 cc (D0.02cc) and was noted to be 6.46 GyE.
The mean left ventricular dose V5Gy is documented in Table 3. This was low in post-BCS proton therapy (i.e., 0.37%) and as well as in post mastectomy proton therapy (i.e., 1.02%).
4. Equivalent dose in 2 Gy (EQD2)
The EQD2 of the mean heart dose ranged from 0.15 to 0.62 GyE. The range for the mean LAD dose was 0.12–8.2 GyE (EQD2), and the max LAD dose was 0.01–23.7 GyE (EQD2).
5. Toxicities and outcomes
One patient had grade 2 dysphagia. Two patients had grade 2 and one, grade 3 dermatitis. The latter occurred in the patient in whom the chest wall contour was not clipped on account of the involvement of dermal lymphatics. The skin reactions required dressing with a hydrocolloid patch and resolved 10 days after completion of therapy. On median follow-up of 12.5 months, the locoregional control an overall survival was 100%.
Discussion and Conclusion
Our data on dosimetric and early clinical outcomes documents the first Indian experience of proton therapy for breast cancer. Our results document consistently low heart and cardiac substructure doses. These are particularly relevant in the background of a high prevalence of cardiovascular risk factors among Indians and other South Asians. These are a significant prevalence of obesity, 44%–72% [22,23] in certain communities, diabetes in >20% of the urban population [24] and a high age-standardized prevalence of hypertension and cardiovascular disease [25]. In our cohort of patients, six patients had cardiovascular risk factors, of which four patients had >1 risk factor.
In addition, patients in India are less likely to be screen-detected, a significant proportion thus requiring anthracyclines and trastuzumab [3]. The additive effect of these cardiotoxic drugs, on the risk of cardiac disease, has been documented in several studies [26].
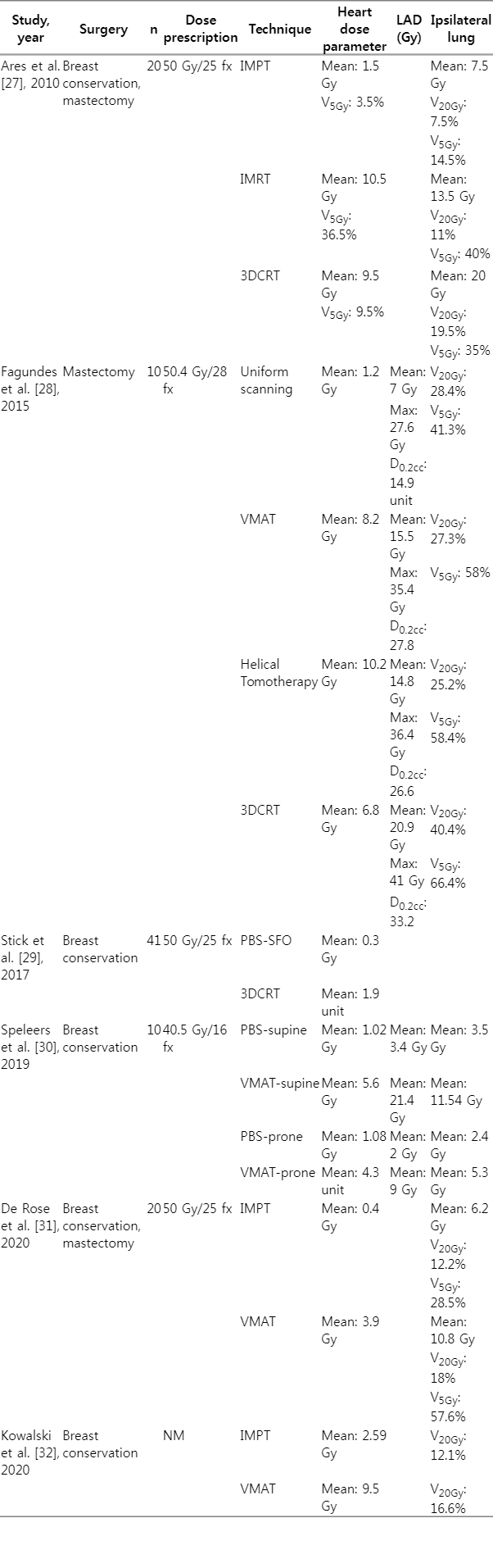
Proton therapy offers dosimetric advantages in cardiac, opposite breast and lung doses over conventional radiotherapy in the treatment of breast cancer, this being first postulated in 1999. The advantage of protons lies in the abruptness of the energy deposition (i.e., Bragg peak) and therefore sparing of distal tissues, like the heart and lungs. Several dosimetric studies have underlined the advantage of proton therapy in reducing the mean dose to the heart in comparison with 3DCRT, IMRT, helical tomotherapy, and VMAT [27-32] (Table 4). Notably, with target coverage remaining adequate and equivalent to photons, the range of reduction in the mean dose to the heart is approximately 73%–90%. The reduction of heart dose by protons is expected to significantly reduce the relative risk of ACEs [12].
This is especially relevant for patients with the cardiovascular risk factors noted above. The correlation of cardiovascular risk factors with a doubling of the risk of ACE has already been elucidated in the landmark study by Darby et al. [12], Jacobse et al. [33], who studied exclusively, the risk of myocardial infarction, also identified that hypertension and BMI ≥30 kg/m2 were the only individual patient-related cardiovascular risk factors significantly associated with an increased myocardial infarction (MI) rate.
1. Mean heart dose
The mean heart dose for left-side breast cancer in our study listed in Table 3 ranges from 0.11 to 1.2 GyE. Notwithstanding internal mammary nodal irradiation in 19 of 20 patients, the mean heart dose in our patients was 0.87 GyE for left-sided and 0.41 GyE for right-sided treatments, respectively (Table 2). Other relevant heart parameters V25GyE, V5GyE, mean dose to left ventricle (LV), LV V5GyE, and mean dose to the LAD are 0.98%, 3.54%, 0.2 GyE, 0.74%, and 2.76 GyE, respectively.
2. Cardiac substructure dose
Thus far, there was a lack of clarity about the relative importance of sparing cardiac substructures, coronary arteries, versus myocardium versus both. This is reflected in the multiplicity of proposed dose constraints and cardiac structures [13,34,35]. Recently, however, relevant dose thresholds have been identified for the LAD and LV. Zureick et al. [36], treating a contemporary cohort of breast cancer patients, found that mean and max doses of LAD were correlated to adverse cardiac events in breast cancer patients. The potential dose threshold identified (by ROC curve analyses) for LAD Dmean was an EQD2 of 2.8 Gy, and for LAD Dmax, an EQD2 of 6.7 Gy for any cardiac event. Similarly, the threshold dose for heart Dmean was an EQD2 of 0.8 Gy for any cardiac event [36]. It is important to note that only 12.5% of patients in this study received adriamycin, and <10% received trastuzumab.
One of the distinct advantages of proton therapy is a reduction in dose to the LAD by as much as 90% compared to photon therapy (Table 4). The mean LAD dose achieved in our left-sided patients was 2.21 GyE, comparable with 2.8–5 Gy reported in various studies [14,36]. In our cohort, the mean and max LAD EQD2 were less than the dose threshold identified by Zureick et al. [36] in 13 of 15 left-sided patients. In one patient, the Dmax for LAD was 36.25 GyE, because of the proximity of the LAD to the chest wall. We used the deep inspiratory breath hold technique for this patient and were able to reduce the Dmax of the LAD to 8.01 GyE.
The LV V5 has been postulated to be a better correlate of cardiac dysfunction than the mean heart dose based on a retrospective study of 910 patients followed up for a median of 7.6 years by van den Bogaard et al. [13]. This parameter has only recently been addressed in published literature and was documented to range from 0 to 3.37% in this series. Abraham et al. [14], prospectively analyzed 181 breast patients, with a median follow-up of 127 months and recorded any cardiac events, viz., any ischemic event, conduction abnormality, congestive heart failure, pericarditis and valvular disease. The authors noted that mean left ventricular dose <5.85 Gy (p = 0.035), V5 <42 cc (p = 0.024) and V10 <38 cc (p = 0.081) reduces additional risk of radiation-related cardiac events to <5% at 10 years. Using proton therapy, our mean left ventricular dose was 0.2 GyE. The absolute V5 volume ranged from 0 to 3.7 cc.
3. Published data and ongoing studies
Clinical data published so far is detailed in Table 5 [17,18,37-44]. The largest cohort has been reported by the group at Massachusetts General Hospital, Boston, USA, with a documented locoregional failure rate of 1.6% at a median follow-up of 55 months in 69 evaluable patients treated with proton therapy [37]. The RADCOMP trial [45] comparing protons with photons in breast cancer patients is accruing patients to determine the margin of benefit, with the end point of reduction in major cardiovascular events. The Mayo Clinic trial (NCT02783690) compares hypofractionated radiotherapy with standard fractionation in patients undergoing post-mastectomy proton therapy [46]. The Danish Breast proton therapy (NCT04291378) is recruiting patients to compare photon and proton radiotherapy for early breast cancer, the primary endpoint being cardiac events at 10 years [47]. We have instituted HYPRO-B, CTRI/2020/11/029415, a prospective registry of patients undergoing hypofractionated proton therapy for breast cancer with the primary objective of determining ACEs at 5 years following hypofractionated proton therapy radiotherapy to the whole breast/chest wall. In addition, we plan to document locoregional control, quality of life, disease-free and overall survival, cardiac function and dosimetric analysis for the latter.
4. Cost-effectivity
We believe that the application of more sophisticated radiation treatment techniques based on better dosimetric parameters, in the absence of or preceding Phase III trials, has many precedents [48-50]. There are concerns about the cost of treatment without evidence of demonstrable benefit in overall survival thus far [51]. Models estimating the cost-effectivity of protons suggesting an advantage in patients with at least one coronary risk factor or a mean heart dose of 5 Gy or more are specific to country-based health systems [52]. In addition, cost-effectivity analyses may not be relevant for the individual patient and do not address benefits accruing from avoiding cardiac interventions besides percutaneous coronary intervention (PCI). Proton therapy may also become less expensive in the foreseeable future with the advent of single-room facilities [53].
The current case series and published data indicate that proton therapy fulfils the sound principles of better sparing of organs at risk with equivalent target coverage in breast cancer.
In conclusion, cardiac, lung and contralateral breast doses consistently documented to increase the morbidity of breast radiotherapy are significantly reduced by proton therapy. Early results of pencil beam scanning-based hypofractionated proton therapy with SIB merit the consideration of this treatment in managing breast cancer.
Acknowledgements
We thank Minnal Mookaiah (Radiotherapy Technologist) and Anusha T (Physician Assistant) for their contribution to this study. We also thank our patients and their families.
Notes
Statement of Ethics
This study was approved by the Institutional Ethics Committee-Biomedical Research, Apollo Hospitals, Chennai, India (IEC Application No. API-I-C-S-004110-20; Protocol No. APCC20203, Breast Cancer Proton Registry HyPro-B). Written informed consent was obtained from participants to participate in the study.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author Contributions
Conceptualization, Nangia S. Investigation and methodology, Nangia S, Burela N. Project administration, Nangia S. Resources, Sharma D, Noufal MP, Patro K, Wakde MG, Burela N, Nangia S. Supervision, Nangia S, Sharma D. Writing of the original draft, Nangia S, Burela N, Sharma D. Writing of the review and editing, Nangia S, Burela N. Software, Noufal MP, Burela N. Validation, Nangia S. Formal analysis, Burela N. Data curation, Burela N. Visualization, Nangia S.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.