Synchronous radiation-induced enterovesical and enterocervical fistulas in carcinoma of the uterine cervix
Article information
Abstract
Radiation-induced fistulas (RIF) are uncommon therapeutic complications of radiotherapy in patients treated for carcinoma of the uterine cervix. Synchronous occurrence of enterocervical and enterovesical fistulas secondary to radiation is extremely rare and previously unreported in the literature. We report a case of synchronous enterovesical and enterocervical fistulas in a patient with carcinoma of the cervix treated using chemotherapy and radiation along with a brief overview of etiopathogenesis of RIF.
Introduction
Radiation-induced fistulas (RIF) are rare, late complications of pelvic irradiation that may occur in cervical cancer patients treated with radiotherapy for locally advanced disease. Vagina, urinary bladder and rectum are the most frequent organs to be involved in radiation induced fistulous communications. Among them, the commonest RIF are the vesicovaginal fistulas with a reported incidence of 1%–8%, followed by enterovaginal, ureterovaginal, and enterovesical fistulas [1-3]. Small bowel involvement in radiation induced fistulas is uncommon and fistulous communications between small bowel and urinary bladder (enterovesical fistulas), and small bowel and cervix (enterocervical fistulas) are extremely rare. We searched PubMed/MEDLINE databases for previous case reports or series, using the keywords “enterovesical fistula and enterocervical fistula”. We could find only a single report of spontaneous enterocervical and enterovesical fistulas published in German language in 1954 [4]. We report a case of synchronous enterovesical and enterocervical fistulas in a patient with carcinoma of the uterine cervix treated using chemotherapy and radiation along with a brief overview of etiopathogenesis of RIF.
Case Report
A 50-year-old woman diagnosed as carcinoma of the uterine cervix, stage IIB was treated with chemotherapy and radiation. Patient underwent external-beam extended-field radiation therapy using conventional four-field box technique (anteroposterior-posteroanterior, right lateral-left lateral). Intracavitary brachytherapy was not given in this patient. Patient received a total radiation dose of 50 Gy in the form of 25 fractions over 5 weeks (5 fractions per week) at the rate of 2 Gy/fraction/day. Concurrent chemotherapy with cisplatin 40 mg/m2 once weekly for 5 weeks was also given. No other abnormalities were noted in the history and patient was asymptomatic after the treatment. A year after chemoradiation therapy, patient developed feculent discharge per urethra and was referred to our institute, a tertiary care cancer center, for further management. Clinical examination and vital signs were normal. On vaginal and rectal examination, induration at cervix was noted. Ultrasound of abdomen and pelvis revealed multiple air foci in a partially distended urinary bladder with a communication between the bladder and ileal loop suggestive of enterovesical fistula (Fig. 1). Computed tomography (CT) of abdomen with oral contrast revealed an ileal loop between the urinary bladder and uterus with passage of contrast into the urinary bladder anteriorly and cervix posteriorly, demonstrating synchronous enterovesical and enterocervical fistulas (Fig. 2). Patient underwent surgery, and intraoperative findings showed interposition of distal ileal loop between the urinary bladder and uterus with adhesion of distal ileal loop to urinary bladder, at about 10 cm proximal to ileocecal junction. Ileal loop was pale, non-compliant and the bowel wall was communicating with both urinary bladder and cervix confirming the diagnosis of synchronous enterovesical and enterocervical fistulas. Laparoscopic diversion ileostomy was performed and the patient recovered. Histopathology of bowel wall did not reveal any malignant cells. Microscopic examination revealed features of chronic radiation damage that included vascular changes, atypical fibroblasts and eosinophilic infiltrates, crypt distortion due to fibrosis of the lamina propria, along with fibrosis of the submucosa, muscularis propria and subserosa of bowel wall.

Transabdominal ultrasound image reveals partially distended urinary bladder (UB) communicating with hypoechoic ileal loop (IL) through an irregular track of hyper-echoic air (thick arrow) suggestive of enterovesical fistula. Presence of air in the UB, seen as hyperechoic foci (thin arrow) is an indirect sign of vesical fistula.
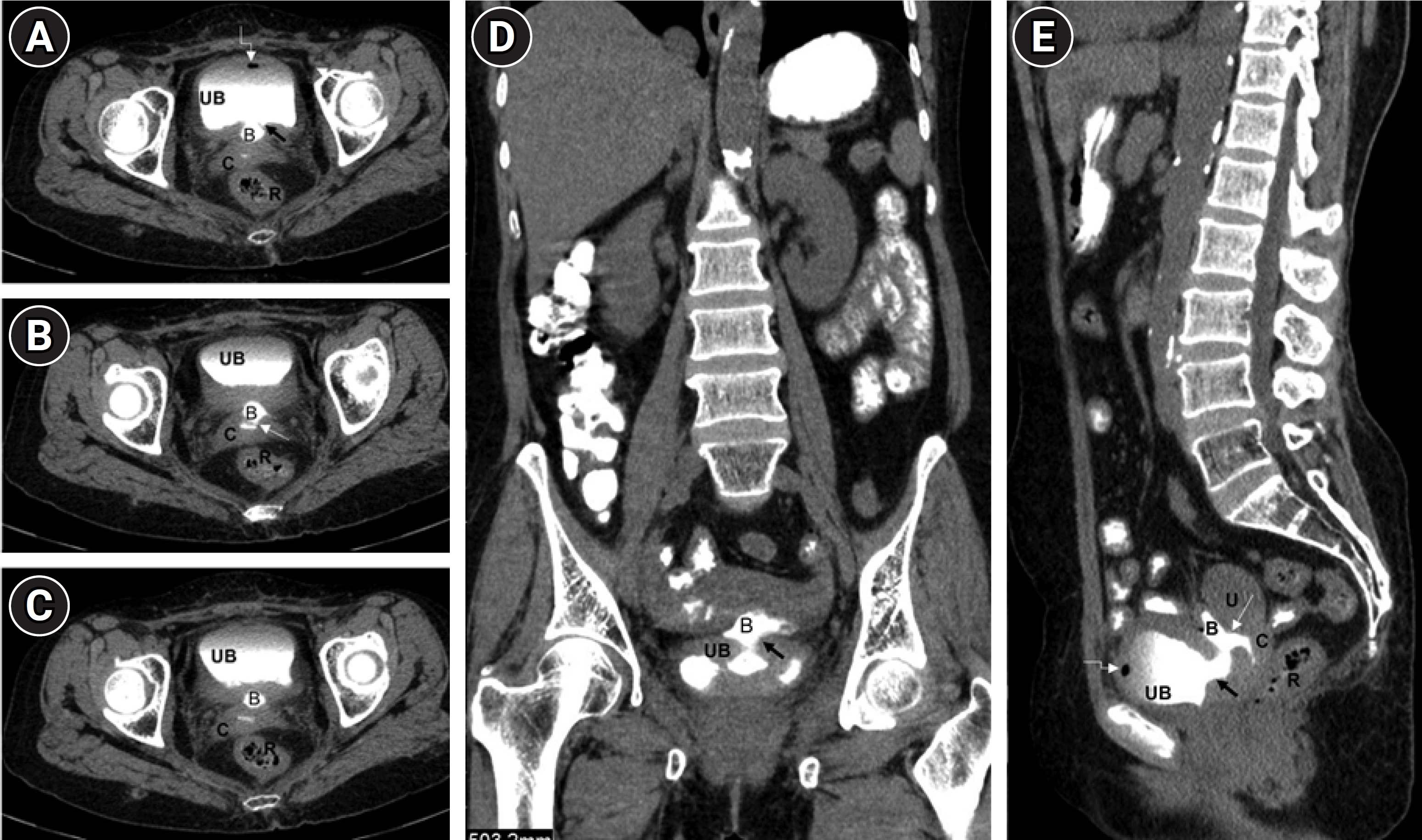
(A–E) Axial and reconstructed coronal and sagittal computed tomography images of abdomen and pelvis with oral contrast show enterovesical fistula (thick black arrow) between the ileal loop (B) and urinary bladder (UB), and enterocervical fistula (thin white arrow) between the ileal loop (B) and cervix (C). Oral contrast is seen in the bowel loops in the abdomen, bladder, cervix, and the ileal loop (B) interposed between the UB and uterus (U). Air focus seen in the bladder (white elbow arrows) is an indirect sign of vesical fistula. Normal rectum (R) is seen posteriorly in the images.
Discussion
RIF are uncommon and late therapeutic complications of malignancies and are associated with several predisposing factors. Systemic conditions causing microvascular ischemia such as diabetes, atherosclerosis, hypertension, and smoking are also linked to the acceleration of fistulation process [5]. The epithelial lined gastrointestinal and genitourinary organs are sensitive to radiation and are highly susceptible to radiation injury. Though small bowel is more radiosensitive than the large bowel, occurrence of fistulas is rare in small bowel due to its mobility in peritoneum. In cases of small bowel involvement, the terminal ileum, due to its relative fixity, is the most common segment to develop fistulous communications. Radiation injury to the bowel is dose dependent, hence increased incidence of fistulas is seen with higher doses of radiation and large field of irradiation. Timing of radiation is also important, as postoperative radiation is more lethal than preoperative radiation [5]. Simultaneous chemoradiation therapy, though is the standard nonsurgical treatment for cervical cancer, concurrent chemotherapy increases the early and late toxic effects of radiation including fistula formation [5-7].
Prior abdominopelvic surgeries causing adhesions between the bowel loops and adjacent organs in the pelvis can lead to inadvertent inclusion of bowel loops in the radiation field, predisposing to fistula formation [5]. Increased incidence of fistulas is also seen in patients with history of hysterectomy due to the absence of uterus that acts a protective barrier between the pelvic organs. Hence, most of the cervical cancer treatment protocols, except for stage II cancers with high-risk features, include either only radiotherapy or hysterectomy but not both [3].
The underlying etiopathogenesis of RIF is progressive chronic ischemia occurring due to endarteritis obliterans resulting in necrosis and fibrosis with loss of tissue planes leading to the development of fistulas [1,6]. Radiation-induced damage to the microvasculature of pelvic and abdominal organs initially present with acute symptoms of cystitis, enteritis, and proctitis and further progress to chronic complications like formation of strictures, abscesses, and fistulas [2,8]. Post-radiation fistulas occur late in the course of disease due to chronic toxic effects of radiation. The mean duration of occurrence is 2–3 years after radiotherapy, though cases have been reported from 6 months to 20 years after radiotherapy [9].
Post-radiation fistulas associated with cervical malignancy are usually multiple, large, and complex. Spontaneous closure is unlikely in these cases, and they invariably need surgical intervention. Bowel loops adjacent to the segment involved in the fistula formation may appear normal on gross examination. Radiation-induced damage to the intestinal microvasculature is difficult to appreciate clinically, there by presenting a challenge in assessing the viability of the tissues adjacent to fistula and in delineating the extent of radiation injury. RIF are often refractory to treatment and the failure rate of surgical repair is high due to the presence of nonviable ischemic tissue leading to anastomotic dehiscence and leaks [3,10].
Accurate diagnosis and appropriate management are the key to quality life in cervical cancer patients with radiation induced fistulas. Radiological imaging with ultrasound, CT, and magnetic resonance image (MRI) plays a crucial role in suspecting and confirming the diagnosis of fistulas. On ultrasound, the presence of a hyperechoic tract within a hypoechoic neoplastic mass described as "air contrast sign" and "ring down" artifacts are useful in detecting fistulas [11]. In suspected cases of RIF, CT with oral/rectal contrast is the imaging modality of choice as it excellently depicts the fistulous tracts, presence of malignant mass, air and/or contrast in inappropriate location [7,12]. MR imaging with its superior soft-tissue resolution may be useful in demonstrating the nonviable ischemic tissue and contrast-enhanced MRI using intravenous gadolinium can differentiate radiation-induced fibrosis which does not enhance from residual/recurrent malignancy [6].
The etiopathogenesis of the unusual enteric fistulas in the present case could be attributed to multiple factors such as adhesion of bowel loop to the urinary bladder, applying extended field radiation using conventional four-field technique that included the bowel loop within the radiation field and administering concomitant chemotherapy. Targeted radiotherapy utilizing intracavitary brachytherapy or intensity-modulated radiation therapy, prior imaging to rule out anatomical variations and appropriate contouring of radiation field are few measures useful in reducing the radiation damage to target organs and adjacent structures, thereby reducing the occurrence of fistulas.
In patients treated for cervical malignancies, fistulous communications can develop between adjacent organs in the pelvis due to either radiation injury or recurrence of malignancy. Hence, in cervical cancer patients with a past history of radiation, detection of a fistula warrants comprehensive clinical and radiological evaluation including biopsy, for appropriate management, as nearly one-third of the patients develop recurrence, typically within 18 months of therapy [2,13].
Notes
Statement of Ethics
Written informed consent was obtained from the patient for publication of this case report.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Funding
None.
Author Contributions
Conceptualization, Mandava A; Investigation and methodology, Raju K; Formal analysis, Mandava A, Koppula V, Kandati M; Data curation, Mandava A, Koppula V, Kandati M; Writing of the original draft, Mandava A; Writing of the review and editing, Mandava A, Koppula V, Kandati M, Raju K.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
