Treatment outcome of postoperative radiotherapy for retroperitoneal sarcoma
Article information
Abstract
Purpose
To evaluate the treatment outcome and prognostic factor after postoperative radiotherapy in retroperitoneal sarcoma.
Materials and Methods
Forty patients were treated with surgical resection and postoperative radiotherapy for retroperitoneal sarcoma from August 1990 to August 2008. Treatment volume was judged by the location of initial tumor and surgical field, and 45-50 Gy of radiation was basically delivered and additional dose was considered to the high-risk area.
Results
The median follow-up period was 41.4 months (range, 3.9 to 140.6 months). The 5-year overall survival (OS) was 51.8% and disease free survival was 31.5%. The 5-year locoregional recurrence free survival was 61.9% and distant metastasis free survival was 50.6%. In univariate analysis, histologic type (p = 0.006) was the strongest prognostic factor for the OS and histologic grade (p = 0.044) or resection margin (p = 0.032) had also effect on the OS. Histologic type (p = 0.004) was unique significant prognostic factor for the actuarial local control.
Conclusion
Retroperitoneal sarcoma still remains as a poor prognostic disease despite the combined modality treatment including surgery and postoperative radiotherapy. Selective dose-escalation of radiotherapy or combination of effective chemotherapeutic agent must be considered to improve the treatment result especially for the histopathologic type showing poor prognosis.
Introduction
Retroperitoneal sarcoma (RPS) is a rare tumor with approximately 5 to 15% of entire soft tissue sarcomas [1,2]. Diagnosis on many RPS are delayed due to absence of specific early subjective symptom, thus patients visit the hospital mainly complaining abdominal pain or dyspepsia as the enlarged tumor compresses adjacent organs [3]. For this reason, many cases found in more than half of patients with RPS larger than 10 cm at the time of diagnosis but with rare distant metastasis [4,5]. The most effective treatment for RPS known so far is a surgical resection [6-9]. It has been known that complete resection of RPS having sufficient resection margin through radical excision or en bloc resection can improve survival rate [2,3,10,11]. However RPS present difficulties in their complete resections because of the large tumor mass and the complexity of the anatomy where the tumor is located as major organs as well as blood vessels and nerves are distributed inside such as kidney, urinary tract, adrenal gland, small intestines. According to some reports, the complete resection requires also resection of more than one organ approximately in 70 to 90% of patients [3,11,12]. Moreover, even if the surgical resection is to be performed, the prognosis would be poor with 5-year local control rate with the range of 40 to 71% and 5-year survival rate as being 51 to 60% [10,13,14].
For RPS, the death from local recurrence is more prevalent than that from distant metastasis therefore, it is important to decrease local recurrences [5,7,13]. As one of efforts to reduce the local recurrences, the preoperative and postoperative radiotherapy are being tried and some retrospective studies had reported on the local control effects of radiotherapy [4-6]. But their effectiveness is controversial. Thereby the radiotherapy is still being performed in some patients only. Therefore we had conducted the retrospectively analysis on local control rate, survival rate as well as prognostic factors of the patients with RPS, who underwent the postoperative radiotherapy in order to identify on the role of radiotherapy in treating RPS.
Materials and Methods
Forty patients with RPS underwent the postoperative radiotherapy after complete resection between August 1990 and August 2008. The criteria of study subjects inclusion is as follows: 1) patients whose ages were ≥20 years old when diagnoses were made, 2) patient underwent complete resection, 3) patients with no distant metastasis at the time diagnoses were made, 4) patients received the postoperative radiotherapy with dose ≥30 Gy, and 5) patients who had been followed-up over 1 year as out-patient. Other than aforementioned patients, those with gastrointestinal stromal tumor or those with leiomyosarcoma in uterus were excluded. The histological grades were classified into the low grade and the high grade. The size of tumor was defined using the longer diameter of tumor on the axial images taken from the examination with abdominal computed tomography (CT) or magnetic resonance imaging (MRI).
The postoperative radiotherapy was performed as 3-dimensional computerized dosimetry by mainly using 15 MV X-ray. Depending on the resection margins, when the complete resection was achieved, the radiotherapy was performed with total dose from 45 to 50 Gy at 1.8 Gy daily for 5 times a week. When the complete resection was not achieved, the additional radiotherapy was performed at 1.8-2 Gy daily for 5 to 10 times on the area suspected for any remaining tumor.
Gross target volume was defined with either the remaining postoperative mass or the surgical resection margins referring to the preoperative imaging examination whereas clinical target volume was defined with either redundancy of 3-5 cm at the resection range of tumor or with consideration of anatomical risky areas, and except any special cases, the regional lymph nodes were deliberately excluded. Planning target volume was defined by adding 1-1.5 cm to clinical target volume.
Local recurrence was defined as the case of recurrence within the region surgically dissected or the region treated by radiation. In addition, all of recurrences outside the radiation field including retroperitoneal recurrence or abdominal recurrence were considered as distant metastases.
The survival period was defined as from the day of surgery to the date of death or the date of final follow-up observation, and the disease-free survival period was defined as from the day of surgery to the date of initial local or distant recurrence. Kaplan-Meier method was used for analysis of survival rates and Cox Proportional Hazards Model was used for significance verification and prognostic factor assessment. For statistical processing, the study had used SPSS ver. 12 (SPSS Inc., Chicago, IL, USA) program, with significance level defined within 0.05. The prognostic factors of tumor had included gender, location and size of tumor, histological grades, histological subtypes, surgical resection margins, radiotherapy timing, volume of irradiation dose, and chemotherapy.
Results
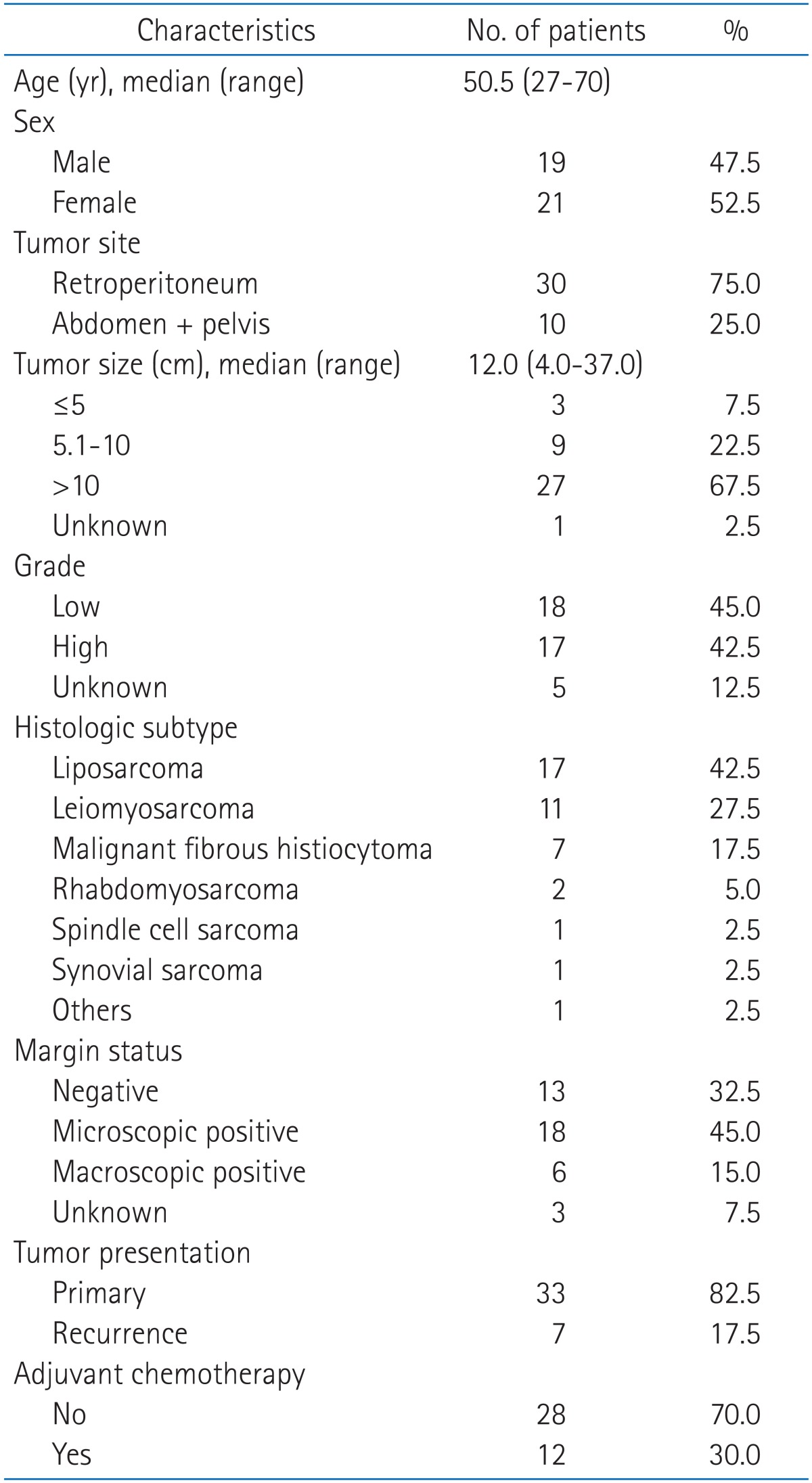
The follow-up period of all patients was ranged from 3.9 to 140.6 months (median, 41.4 months). The most common histological subtype diagnosed was liposarcoma as being found from 40% of the entire patients followed by leiomyosarcoma (27.5%) and malignant fibrous histiocytoma (17.5%). Seven patients had received the radiotherapy after surgical resection of locally recurred tumor. Any other clinical features of patients are as shown in Table 1.
Among 12 patients who underwent the chemotherapy, 3 patients had received the chemotherapy after undergoing the radiotherapy while 9 patients had received the chemotherapy for 3 to 6 times before undergoing the radiotherapy. The median radiotherapy period was 44.5 days (range, 29 to 55 days) and the median of total irradiation dose was 55.9 Gy (range, 36.0 to 65.0 Gy).
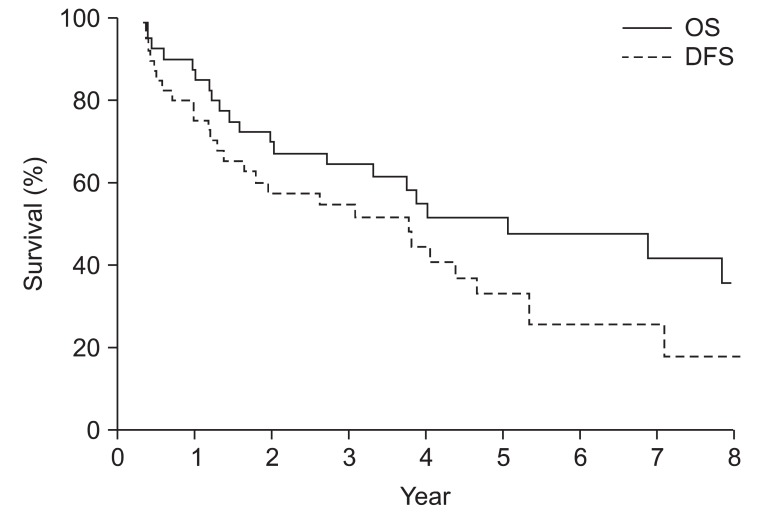
Nineteen patients (47.5%) were alive at the time when analysis had been performed and 14 patients of them (35%) were with the absence of metastatic disease. Twenty-one patients (52.5%) had died, and among them 16 patients (42.0%) had died of the recurrence of disease. Five-year survival rate of all patients was 51.8%, while 5-year disease free survival was 31.5% (Fig. 1).
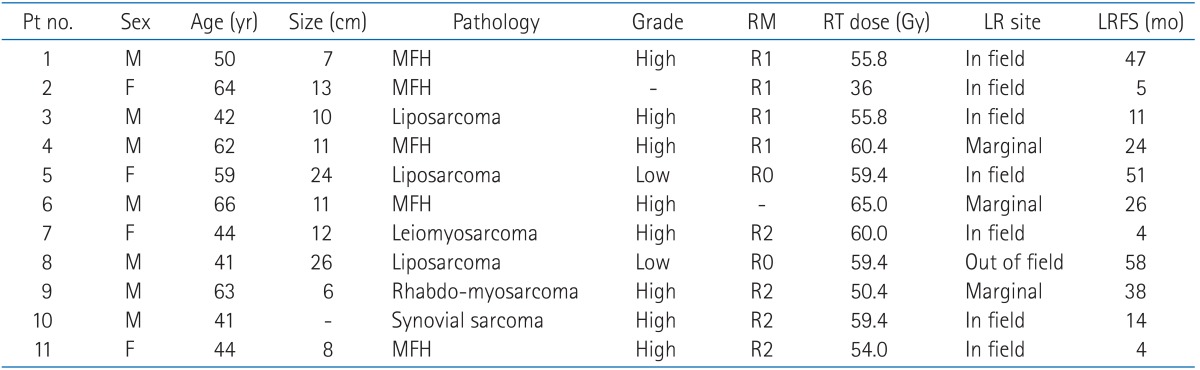
Local recurrences were found from 11 patients (27.5%) in total within the period range from day of surgery to the onset of local recurrence as 3.5 to 58.4 months (median, 14.2 months). Distant metastases were found from 21 patients (52.5%) with the period range from the day of surgery to the onset of distant metastasis as 3.5 to 89.6 months (median, 15.5 months). Five-year local control rate and 5-year distant metastasis free survival rate were 61.9% and 50.6%, respectively. Five patients had been found with local recurrence only, 15 patients were found with distant metastasis only, and 6 patients were found with both of local recurrence and distant metastasis. Among 6 patients who had both of local recurrence and distant metastasis, 1 patient had been found with onset of local recurrence after 18.3 months of distant metastasis while 1 patient had been found the onset of distant metastasis after 7.9 months of local recurrence. Remaining 4 patients were found with distant metastasis diagnosed together with onset of local recurrence. The radiation fields of 11 patients with local recurrences were reviewed. Seven of them had the recurrence inside the radiation field whereas 3 of them had the recurrences at adjacent area of the radiation field. One of them had the local recurrence inside the surgery margin but it was external area of the radiation field. The clinical features of these patients are as shown in Table 2. Among 21 patients to whom distant metastasis had diagnosed, 8 patients had retroperitoneal and abdominal cavity metastases outside radiation field and resection site, 7 patients had pulmonary metastases, 4 patients had hepatic metastases, 3 patients had shown metastases to abdominal organs except the liver, and 2 patients had shown metastases to femur. Among these, 3 patients had been found with distant metastases to more than 2 sites.
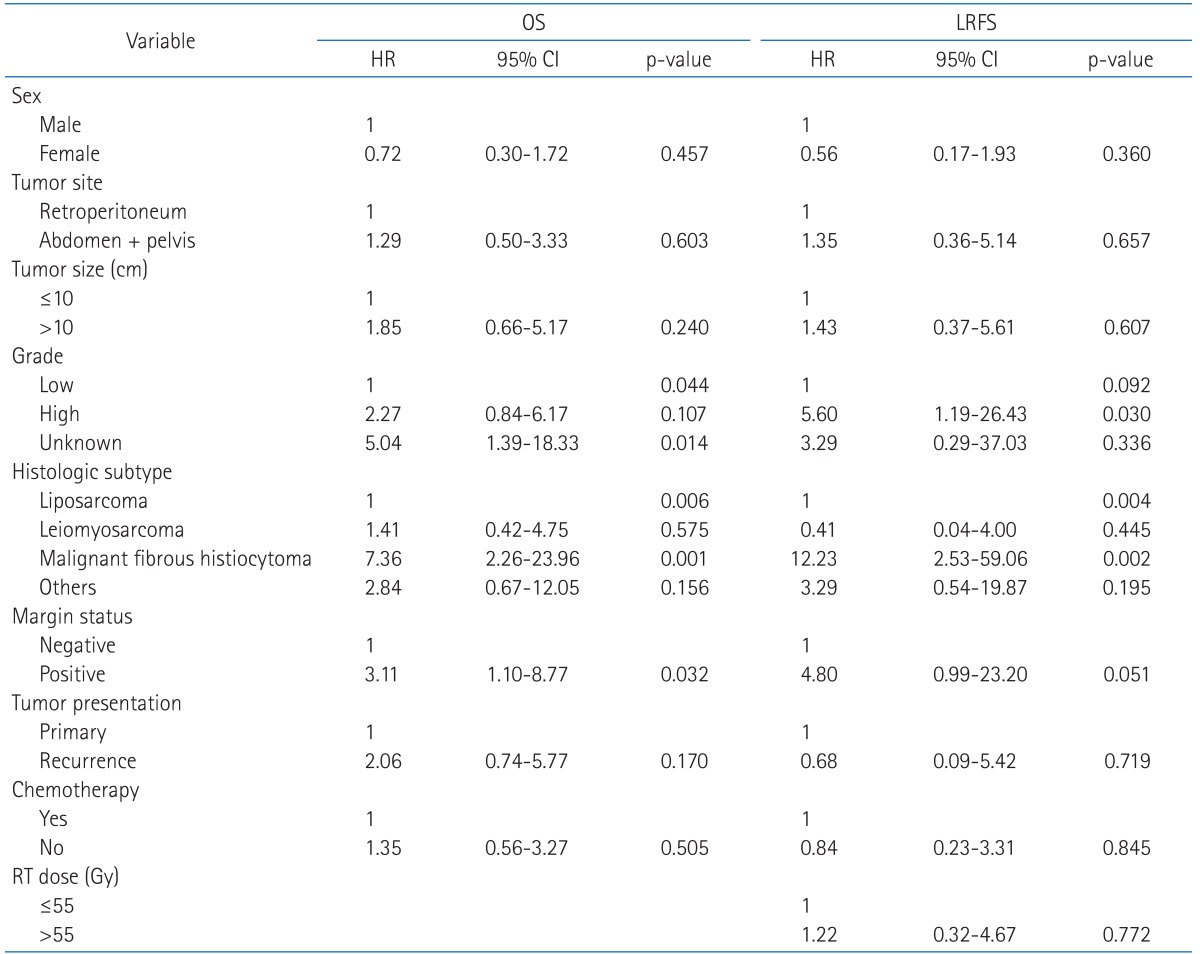
The results of a univariate analysis on prognostic factors had shown that histological grades (p = 0.044), histological subtypes (p = 0.006) (Fig. 2A), and the resection margin (p = 0.032) were the factors having significant effects on survival rates. The low-grade sarcomas had shown better prognosis compared to the high-grade sarcomas or the tumors with grades unidentifiable. Liposarcoma also had shown better prognosis compared to other histological subtypes. On the contrary, the results presented that malignant fibrous histiocytoma decreased the survival rates with statistical significance (p = 0.001). Histological subtypes (p = 0.004) (Fig. 2B) was identified as the factor having significant effects on the local control rates. Likewise with the prognostic factors of survival rates, liposarcoma was identified as the factor improving the local control whereas malignant fibrous histiocytoma was identified as the factor raising the local recurrence (p = 0.002). The resection margin had shown a tendency of factor that had effects on the local control rates (p = 0.051) (Table 3). Histological grades (p = 0.006), histological subtypes (p = 0.009) (Fig. 2C) were identified as the prognostic factors for distant metastasis.

Survival rates according to histologic type. (A) Overall survival rate according to histologic type. (B) Local recurrence free survival rate according to histologic type. (C) Distant metastasis free survival rate according to histologic type. MFH, malignant fibrous histiocytoma.
Discussion and Conclusion
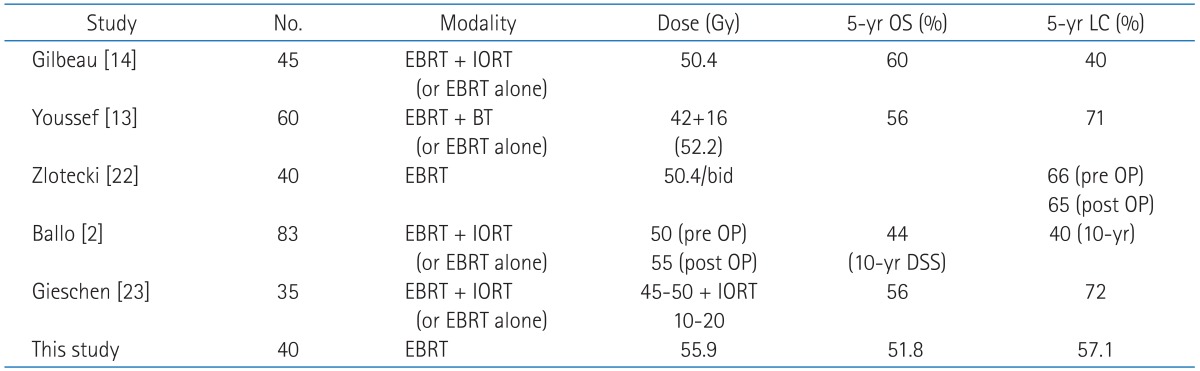
Two prospective studies had verified the local control effects of radiotherapy on the extremity sarcomas which is the most common type of soft tissue sarcomas [15,16]. Nonetheless, the radiotherapy in RPS is still subjected to debates. But, from various retrospective studies, its role had reported on the rising of local control rates through the preoperative radiotherapy and postoperative radiotherapy [4-6,8,9,11]. Converse to the extremity soft tissue sarcomas, in which the presence of distant metastasis has the largest effects on the survival rates [17], in RPS in which the local failure had been closely related to the survival rates [5,7,18], the rising of local control rates can make it possible to expect the improving of the survival rates [5,11,19]. However, it should be noted that there are also a lot of skeptical opinions on the radiotherapy. The underlying cause of such skeptical opinions is that there have been no prospective study available up to now and it is very rare practically to see that the improving of local control by the radiotherapy had been led to the rising of survival rates [5,6,9]. The fact that radiotherapy is being performed in approximately 20-30% of all patients who underwent the surgical resection indicates that such opinions are really existing substantially [5,8,12,20,21]. In such setting, those studies reported the results of radiotherapy were conducted in rather small sample population around 37 to 86 patients [2,13,14,22,23]. Five-year local control rates of them were in the range of 40-71%, presenting similar levels to the results of this study (Table 4).
This study was conducted only in the patients who underwent the postoperative radiotherapy. Currently there is no optimal time of radiotherapy for RPS but the postoperative radiotherapy is being performed in more than half of patients [5,13,20,21,24]. The postoperative radiotherapy is widely used for its advantages that it does not delay the surgery, and it can provide selective treatment in the high risk group depending on the biopsy results or when the complete resection is failed [25]. Therefore, it is performed mainly in the cases of high grades, incomplete resection or that could not obtain sufficient resection margin [8,19]. However, according to the study report of Zhou et al. [8], the radiotherapy was performed mainly American Joint Committee on Cancer (AJCC) stage II and III whereas the local control effects of radiotherapy was presented significantly from patients of stage I only. Tseng et al. [20] also had reported that the local control effects of radiotherapy had been presented more notably from the medium grade than the high grade, indicating further studies are required on the patient group who responded to the radiotherapy effectively. The preoperative radiotherapy is more advantageous as it can more clearly define the treatment region than the postoperative treatment and as the tumor pushed small intestine out to peripheral sides so that gastrointestinal complication during the radiotherapy can be minimized [26,27]. Also, it can reduce the size of tumor before surgery enabling the complete resection so as to raise the local control rates [19]. In fact, according to the study of Ballo et al. [2], 33 patients had received the postoperative radiotherapy among 83 patients who had received both of surgery and radiotherapy, and 5 (23%) of those 33 patients had onset of gastrointestinal complications, whereas no complications had incurred in 50 patients who had received the preoperative radiotherapy, reporting that there was no difference in the local control rates between two treatment groups. Zlotecki et al. [22] also reported that among those patients who has undergone both surgery and radiotherapy, 15 patients had received the postoperative radiotherapy and 7 (47%) of them were identified with local recurrence whereas 4 (16%) were identified with local recurrence out of 25 patients who had received the preoperative radiotherapy, implicating the effects of preoperative radiotherapy in improving the local control. However the most studies were included in small sample sizes, therefore further studies would be required for identified the effective radiotherapy timing.
The radiation dose being used in the RPS is approximately 40 to 50 Gy (Table 4). In case of the extremity soft tissue sarcomas, it is recommended to perform the initial radiotherapy dose range between 40-50 Gy, and then perform additional radiotherapy dose range between 16-20 Gy after reducing the radiation field [28]. However, RPS is practically difficult to irradiate over 60 Gy, taken the potential complications at the surrounding major organs such as stomach, kidney, and small intestine into consideration [2]. In particular, because the small intestine is dislocated when performing the postoperative radiotherapy, the complication rates get even higher. Nevertheless, some studies report that it is possible to expect higher the radiation dose is raised the local control rates. Fein et al. [29] reported 2 (25%) of 8 patients who had received the radiotherapy with dose >55.2 Gy were identified with local recurrence whereas 5 (38%) of 13 patients who had received the radiotherapy with dose ≤55.2 Gy were identified with local recurrence. With this report they recommend the radiation dose ≥55.2 Gy. Tzeng et al. [30] also had performed the preoperative radiotherapy in 16 patients with radiation dose up to 57.5 Gy by intensity modulated radiation therapy, which had resulted in comparatively good outcome with the 2-year local control rate of 80%, thereby it would be required to have further study on optimal radiation dose.
Some institutions perform the intraoperative radiation therapy (IORT) to increase the radiation dose while to minimize the radiation dose of small intestine. Sindelar et al. [31] had compared the local control rates between 15 patients who had received IORT (20 Gy) combined with the external-beam radiation therapy (35-40 Gy) and 20 patients who only received the external-beam radiation therapy (35-40 Gy + 15 Gy). They reported the differences in the date of local recurrence free survival that those patients who underwent IORT was >127 months while those who did not undergo IORT was 8 months. Also Gieschen et al. [23] had performed the preoperative radiotherapy at dose range of 45-50 Gy in 37 patients, thereafter performed IORT only in 20 patients. They has shown better results by presenting the local control rates as 83.3% and the overall survival rate as 74.4% in patients who received IORT among those underwent the complete resection, in comparison to the patients who did not receive IORT (Local control rates, 60.6%; Overall survival rate, 30%). However, with additional IORT, it shows tendency that gastrointestinal complications are reduced but urological and neurological adverse effects are increased [23,31]. Therefore, there should be sufficient further studies on those adverse effects for additional IORT.
In this study, the margins of surgical resection, histological grades and subtypes were identified as the prognostic factors that have effects on the survival rates and the local control rates. Many studies had already reported that these three factors are related with the prognosis [4-7,11,13,22]. Among them, it was identified that liposarcoma as the most commonly encountered histological subtype of RPS has better prognosis in comparison to other histological subtypes from several studies [3,5,6,20]. Liposarcoma is characterized with more frequent local recurrences but with rare incidences of distant metastasis [7,18]. The reason for good survival rates in spite of frequent local recurrences is considered as that it is possible to increase the survival rates by the salvage surgery after recurrence [32]. Leiomyosarcoma and malignant fibrous histiocytoma have poorer prognosis compared to liposarcoma, having higher prevalence of distant metastasis than local recurrence [3,11]. In this study, the malignant fibrous histiocytoma had shown very poor prognosis both in the local recurrence and the survival rates. It might be possible to find the underlying cause of such poor prognosis through reports saying the malignant fibrous histiocytoma is a dedifferentiated or undifferentiated liposarcoma [33,34].
From the results of this study, even the surgical resection and the adjuvant radiotherapy could not bring satisfactory treatment outcomes in connection to the survival rates as well as the local control rates for the RPS. The study also indicates that further studies would be required to identify methods of increasing the radiation dose selectively for the histological subtypes with low local control rates and survival rates and also on effective combination with chemotherapy.
Acknowledgments
This study was supported by a grant (2009-472) from the Asan Institute for Life Sciences, Seoul, Korea.
Notes
No potential conflict of interest relevant to this article was reported.