Reviewing the potential role of radiation therapy in gallbladder cancer: an update
Article information
Abstract
Gallbladder cancer is a highly malignant disease with a poor prognosis. It is the most common cancer of the biliary tract pathway. Although surgery remains the treatment of choice for early-stage disease, majority of the patients presents in locally advanced, unresectable and metastatic stage of the disease. Radiotherapy and chemotherapy thus form an integral part of management for these locally advanced staged patients. The role of radiation though has been advocated in gallbladder cancer, majorly in the adjuvant setting, its role in neoadjuvant and palliative settings remains in an evolving phase. The article thus aims to review and update the existing literature regarding the role of radiation therapy in gallbladder cancer.
Introduction
The gallbladder is a small pear-shaped organ that lies underneath the liver and stores bile. Despite being a small organ there is a high chance of malignancy reported. The absence of the serosa layer, proximity to critical adjoining structures, and easy extension to lymphatics makes it vulnerable for early dissemination. Often, patients present in an advanced stage of the disease, with disseminated metastasis being reported in the range of 65% to 82%, for hematological metastasis and 91% to 94% for lymphatic metastasis, respectively [1,2]. Although its incidence in Western countries is less, it is quite prevalent in Asian counties with a high prevalence seen amongst obese females with a personal or family history of gallstones and ill-defined genetic variants [3]. According to GLOBOCAN 2020 data [4], gallbladder cancer (GBC) is the 23rd most incident but 20th most deadly cancer worldwide.
Depending upon the stage of the disease, surgery, radiotherapy (RT), and chemotherapy are the modalities of treatment used for GBC. Although surgical treatment remains the only curative treatment for early-stage GBC, most of the patients present in locally advanced or metastatic stages of the disease, requiring RT and chemotherapy as an adjunct to a definitive modality or as palliative therapy.
With the advancement in technology, RT techniques have evolved over the years from two-dimensional (2D) techniques to intensity-modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT). Lately, not much about its role in GBC have been reviewed. The present article thus aims to review the role of RT as used in the past and its usage during the present era.
Role as Adjuvant Therapy
In GBC, the outcomes are poor, even after complete resection with high rates of both local and distant relapses. The relapse rates are high, especially in ≥T3, and in node-positive disease [5,6]. Adjuvant therapy is indicated in patients with completely resected muscle-invasive disease, node-positive disease, and margin-positive GBC.
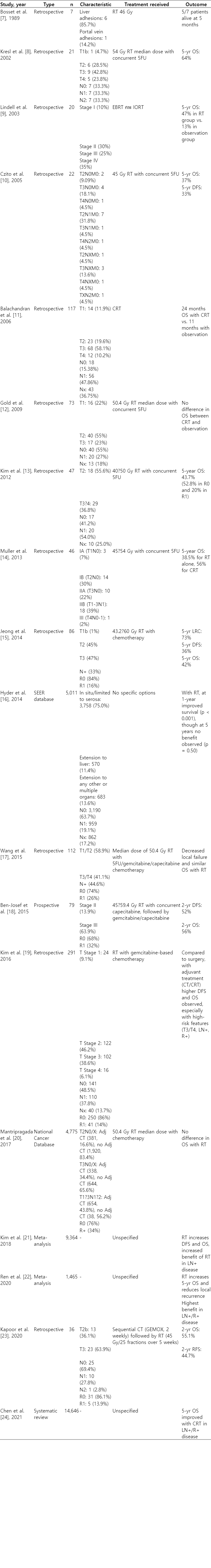
Various studies have advocated the role of adjuvant RT, as shown in Table 1 [7-24]. The benefit of the adjuvant RT was first reported by Bosset et al. [7]; five patients out of seven were alive after a median follow-up of 5 months in their study. The support for adjuvant therapy is further derived from a few population-based studies and SEER database demonstrating the benefit of chemoradiotherapy (CRT) over chemotherapy alone in T2 or above; or node-positive patients. SWOG 0809 trial [18] published in 2015 has evaluated the role of adjuvant chemotherapy followed by RT in extrahepatic biliary cancers and GBC in a phase II trial. In this trial, patients received gemcitabine injection 1,000 mg/m2 on D1 and D8 and oral capecitabine 1,500 mg/m2 twice daily for 14 days for 4 cycles. This was followed by RT (54–59 Gy to the tumor bed and 45 Gy to the nodal regions) along with concurrent capecitabine 1,330 mg/m2 daily. With a median follow-up of 35 months, overall survival (OS) was 65% (67% in the R0 group and 60% in the R1 group). Though there was no head-to-head comparison with patients receiving chemotherapy alone or patients kept on observation, the local recurrence was 11% in this study, compared to the 16%–30% estimated risk of local recurrence in patients receiving no adjuvant therapy. However, approximately 52% of the patients had developed grade 3 adverse events and 14% had developed grade 4 adverse events [8-20].
Further, in a meta-analysis conducted by Kim et al. [21] and Ren et al. [22], the patients with node-positive and margin-positive disease derived clear survival benefits from adjuvant therapy. Kapoor et al. [23] concluded in their study that sequential CRT without concurrent RT could be a better-tolerated regimen, at the cost of lower survival rates. In a systematic review conducted by Chen et al. [24], the benefit was seen in patients with node-positive or margin-positive status.
Though three-dimensional (3D) CRT is the most common modality used in the RT of gall bladder malignancies in the adjuvant setting, the use of other techniques like IMRT, stereotactic body radiation therapy (SBRT), and proton beam therapy (PBT) is being investigated. Fuller et al. [25] have reported the use of IMRT with ultrasound guidance for GBC and biliary tract carcinomas. The median dose received was 59 Gy with IMRT versus 48 Gy with conventional RT with lower toxicities and higher median survival in the IMRT arm. Further, in a study done by Gedam et al. [26], VMAT plans were generated for patients already treated by IMRT and they concluded that constant dose rate volumetric modulated arc therapy (CDR-VMAT) could be a valid option in patients of GBC planned for RT.
Although the role of brachytherapy is not well established in GBC, Kurisu et al. [27] in their case report highlighted the usage of high-dose-rate intraluminal brachytherapy (HDRIBT) in post-operated patient of GBC with residual disease. They gave HDRIBT (20 Gy/2 fraction) followed by EBRT of 30 Gy/15 fraction at an interval of 2 weeks.
Besides it, the role of SBRT in the adjuvant setting has also been evaluated in some case reports [28,29]. As it has the potential of delivering higher doses to the tumor at a higher dose per fraction while limiting the dose to organs-at-risk (OAR), its role should further be explored by properly conducted clinical trials.
Similar to SBRT, PBT also provides sharp dose gradients with a high dose to the tumor cells and minimal effects on OAR. Makita et al. [30] have treated 28 patients with cholangiocarcinoma and GBC with proton therapy. The median radiation dose was 68.2 Gy radiobiological equivalent (RBE). The 1-year local control, progressive-free survival (PFS), and OS were 67.7%, 29.5%, and 49%, respectively.
Overall, adjuvant RT with or without chemotherapy in its various formats (3DCRT, IMRT, VMAT) plays a crucial role in GBC and is indicated in patients with residual disease, ≥T3 stage, and with node or margin positive status. The role of SBRT and PBT needs further evaluation.
Role as Definitive Therapy
With the advent of modern techniques like image guidance, organ motion management, and adaptive planning, delivering a high dose per fraction ablative RT with a high biologically equivalent dose (BED) has become possible. Few retrospective analyses have analysed the use of definitive RT in unresectable cases of GBC, as depicted in Table 2. A SEER database analysis and a National Cancer Database analysis have stated that the OS is better with the addition of RT to chemotherapy [31,32]. Bisello et al. [33] in a single institute retrospective study, have stated that CRT is a feasible option in cases of unresectable GBC. They had given a median external beam radiation therapy (EBRT) dose of 50 Gy with a BT boost of 14 Gy along with 5-fluorouracil (5FU)/gemcitabine-based chemotherapy.
Very few studies have thus evaluated the role of definitive radiation therapy in GBC. The paucity of patients, poor general condition, and advanced stage at presentation could be some of the possible reasons for it. Although initially considered as a radioresistant tumor, the above-mentioned studies support its usage. Hence trials whenever feasible should be conducted to establish the role of definitive RT.
Palliative Radiotherapy
GBC is usually present in locally advanced or metastatic stages, and thus the treatment offered for such patients is palliative chemotherapy or best supportive care (BSC) only [34]. The goals of palliation usually include relief of pain, jaundice, bowel obstruction, and improving quality of life. Palliative RT is well known to provide relief from local symptoms in patients with various malignancies [35]. The role of palliative RT in GBC is less explored and chemotherapy is the primary palliative therapy.
Eleftheriadis et al. [36] have reported a case of unresectable GBC who has received RT alone. The patient had stable disease at 12 months post-RT. Singh et al. [37] have retrospectively compared BSC alone with chemotherapy and CRT. Fifty patients were included in the analysis. The chemotherapy given was gemcitabine injection 800 mg/m2 and oxaliplatin injection 80 mg/m2 (mGEMOX) given every 2 weekly for 6 cycles and the RT was 30–45 Gy in 10–25 fractions depending on the performance score of the patient. The PFS of patients who received BSC at 18 months was 10%, chemotherapy alone was 28% and with CRT it was 38%.
Transhepatic percutaneous intraluminal brachytherapy using 192Ir has been used as palliative therapy for obstructive jaundice due to bile duct obstruction [38,39]. Thus, the addition of palliative RT to unresectable disease has the potential to improve the PFS and provide symptomatic relief in unresectable GBC. Prospective trials are required to further evaluate the role of palliative RT.
In short, the role of palliative radiotherapy in GBC still needs to be explored. It could be well utilized in this group of patients, especially in patients who are not fit for chemotherapy and presents with jaundice and pain.
Role in Neoadjuvant Therapy
Neoadjuvant therapy improves the rate of resection by downstaging the tumor, improving the operability of the tumor. The role of radiation in GBC in the neoadjuvant setting has been considered to be in a trial setting only (Table 3). de Aretxabala et al. [40] in a prospective study using neoadjuvant CRT in GBC patients, have stated that there was no benefit of using neoadjuvant RT in unresectable GBC and patients had a worse survival with neoadjuvant therapy. Agrawal et al. [41] have prospectively studied the benefit of neoadjuvant CRT in 40 patients of unresectable GBC. RT of 45 Gy in 25 fractions along with concurrent 5FU and cisplatin were given. Neoadjuvant chemotherapy was given before RT if the patient was node-positive. They concluded that neoadjuvant therapy resulted in a 15% resectability rate with a radiological downstaging of liver involvement in 40% of the patients and downstaging of lymph nodes in 67.5%. Engineer et al. [42] prospectively studied 28 patients of locally advanced GBC of T3/T4 with large fixed periportal nodes. In their study, patients were given 57 Gy to the gross tumor and 45 Gy to the clinical target volume (CTV) in 25 fractions along with weekly gemcitabine of 300 mg/m2. Eighteen patients were surgically explored and 14 patients underwent R0 resection. Twenty patients had achieved a complete or partial response. The median OS was 20 months.
High rates of biliary stricture and biliary leak were reported in patients receiving neoadjuvant therapy [43]. There is insufficient data regarding the use of RT in the neoadjuvant setting and the benefit of resectability has been seen in a third of the patients in a pooled analysis of eight studies conducted by Hakeem et al. [44].Perioperative therapy in locally advanced gallbladder cancers (POLCAGB) trial is an ongoing phase 3 trial that is comparing the OS, PFS, resection rates, and toxicities between patients receiving neoadjuvant chemotherapy and neoadjuvant CRT [45]. Though some of the RT studies done in patients of GBC so far support its usage in the neoadjuvant setting, more and more collaborative studies are still warranted.
Conclusion
This article provides an updated overview of the role of RT in GBC in its various formats. As the local failure is high in GBC, RT has a good potential in reducing the local failures in the adjuvant setting. Future usage of advanced techniques might help in providing dose escalation to the tumor site with better sparing of OARs. Definitive RT in patients of unresectable GBC is an area for potential clinical research. Palliative RT too remains investigational, which otherwise could be utilized to reduce the local disease progression and provide symptomatic relief in unresectable cases. Lastly, the use of neoadjuvant therapy to downstage the disease and improve resectability still remains in its preliminary phase which needs further evaluation. Overall, with the paucity of literature supporting the usage of modern techniques of RT in GBC, the role of RT needs to be further enhanced and improved in quality.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.