 |
 |
AbstractPurposeThe details of breast reconstruction and radiation therapy (RT) vary between institutions; therefore, we sought to investigate the practice patterns of radiation oncologists who specialize in breast cancer.
Materials and MethodsWe identified the practice patterns and inter-hospital variations from a multi-center cohort of women with breast cancer who underwent post-mastectomy RT (PMRT) to the reconstructed breast at 16 institutions between 2015 and 2016. The institutions were requested to contour the target volume and produce RT plans for one representative case with five different clinical scenarios and answer questionnaires which elicited infrastructural information. We assessed the inter-institutional variations in RT in terms of the target, normal organ delineation, and dose-volume histograms.
ResultsThree hundred fourteen patients were included; 99% of them underwent immediate reconstruction. The most irradiated material was tissue expander (36.9%) followed by transverse rectus abdominis musculocutaneous flap (23.9%) and silicone implant (12.1%). In prosthetic-based reconstruction with tissue expander, most patients received PMRT following partial deflation. Conventional fractionation and hypofractionation RT were used in 66.6% and 33.4% patients, respectively (commonest: 40.05 Gy in 15 fractions [17.5%]). Furthermore, 15.6% of the patients received boost RT and 53.5% were treated with bolus. Overall, 15 physicians responded to the questionnaires and six submitted their contours and RT plans. There was a significant variability in target delineations and RT plans between physicians, and between clinical scenarios.
IntroductionBreast reconstruction has become very common over the last two decades [1,2]. It significantly improves the quality of life and reduces adverse psychosocial effects following mastectomy [3]. However, the decision regarding breast reconstruction becomes complicated in patients who anticipate to receive post-mastectomy radiation therapy (PMRT) [4]. The majority of radiation oncologists believe that their ability to deliver radiotherapy to the chest wall is challenged by immediate breast reconstruction [5]. Simultaneously, the majority of reconstructive surgeons believe that the cosmetic outcomes of breast reconstruction are negatively affected by PMRT [6,7].
Reconstructions can either be immediate or delayed or a combined approach called delayed-immediate reconstruction [8]. An implant, autologous tissue or a combination of an implant and a flap, can be used for the restoration of the breast mound [9]. All reconstruction approaches have their own pros and cons [10,11]. The techniques available for radiotherapy delivery in patients with breast cancer who have undergone reconstruction have improved over the past decade, which has reduced the challenges in radiotherapy planning that once seemed difficult to overcome. Despite the improvements in both reconstruction and radiotherapy techniques, several issues still require to be answered, such as the type of reconstruction that is the most feasible with PMRT, the timing of reconstruction relative to PMRT, and optimization of radiotherapy to minimize treatment-related complications without compromising the oncological and cosmetic outcomes.
The practice patterns may vary between institutions regarding the reconstruction type and radiotherapy planning and delivery. However, there are no standard protocols or guidelines in clinical settings. Therefore, the aim of this study was to investigate the practice patterns of PMRT in breast reconstruction in Korea.
Materials and Methods1. Ethical statementAfter approval from the review board of the Korean Radiation Oncology Group (KROG 18-04) and Severance Hospital Institutional Review Board (No. 4-2017-0931), a retrospective multi-center observational study and a dummy run study were conducted in patients with breast cancer who received RT and underwent breast reconstruction to identify the practice patterns.
2. Observational studyThe inclusion criteria were as the following: histologically proven breast cancer, non-metastatic disease, female sex, and breast reconstruction following mastectomy and subsequent adjuvant RT between 2015 and 2016. The reconstruction rate has increased since 2015 after reimbursement by the Korean National Insurance Service and we surmised that it was actively performed during this period. Patients who underwent bilateral mastectomy for bilateral breast cancer or were male sex, or lost to follow-up were excluded. The medical charts of the patients were collected and retrospectively reviewed after approval from each participating center.
The following parameters were analyzed: age, body mass index, smoking history, history of diabetes, clinical T and N stages, multicentricity, systemic therapy, mastectomy (standard, skin-sparing, and nipple-sparing), resection margin (clear, close, and positive), reconstruction sequence (one-stage vs. two-stage), reconstruction timing (immediate vs. delayed), reconstruction options (autologous-based vs. prosthetic-based), reconstruction material at the time of RT (tissue expander, implant, transverse rectus abdominis musculocutaneous flap, deep inferior epigastric perforator flap, latissimus dorsi flap, and others), bilateral reconstruction, operation time, RT technique (three-dimensional conformal, field-in-field, step-and-shot intensity-modulated radiotherapy, and volumetric arc therapy), RT dose/fraction, estimated maximum dose in chest wall on RT planning system, chest wall boost RT, bolus material used, and use of regional RT (Table 1).
3. Dummy run studyThe institutions participating in the Division of Breast Cancer, KROG were invited to participate in the present dummy run. They were requested to answer questionnaires (Supplementary A) regarding the infrastructural information, which included computed tomography (CT) simulation, radiation treatment planning (RTP) system, RT treatment details, and quality assurance (QA) activity for the RT machine. CT images from one anonymized patient was provided as a representative case with five different clinical scenarios (cases 1â5) (Supplementary Fig. S1). The physicians from the participating institutions downloaded these CT images from a website and registered them in their own RTP systems; subsequently, they designed RT treatment plans for each clinical scenario. The target range, dose prescription, treatment technique, and beam information were obtained through the questionnaire. RT files in the Digital Imaging and Communications in Medicine (DICOM) format for the structure sets and radiation doses were submitted along with the questionnaires.
Results1. Observational studyOverall, 314 patients treated with PMRT for reconstructed breasts between 2015 and 2016 at the 16 institutions were included. During the same study period, approximately 1,105 patients were referred for PMRT. Table 2 and Fig. 1 present the details of the reconstruction treatments. Most of the patients (99%) underwent immediate reconstruction. One-stage or autologous reconstruction was more frequent than two-stage or prosthetic reconstruction when PMRT was administered. A variety of materials were used for the reconstruction. The most commonly used material was tissue expander (36.9%) followed by TRAM flap (23.9%), silicone implant (12.1%), and a combination of tissue expander and silicone implant (11.2%). When tissue expander was used in prosthetic-based reconstruction, most patients (39.2%) received PMRT after partial deflation. Table 3 presents the details of radiotherapy. Conventional fractionation RT was used in 66.6% of the patients, while hypofractionation was used in 33.4% of patients (commonest: 40.05 Gy in 15 fractions [17.5%]). Additionally, 15.6% of the patients received boost RT and 53.5% of the patients were treated with a bolus.
2. Dummy run and questionnaireOverall, 15 physicians responded to the questionnaires and six physicians submitted their contours and RT plans (Fig. 1). According to the questionnaires, the prescribed dosage varied between physiciansâ. Generally, conventional fractionation with 50â50.4 Gy and over 25â28 fractions was the commonest practice. In a case where a patient was diagnosed with initial clinical internal mammary node metastasis (case 3), one physician responded with prescription of boost dose of 10 Gy in 5 fractions to the internal mammary node after 50 Gy in 25 fractions. Another physician responded with a total dose of 52.8 Gy in 16 fractions with simultaneous integrated boost technique to the internal mammary node. In a case where a patient presented with positive surgical resection margin (case 5), one physician responded with prescription of 54 Gy (Fig. 2). In the questionnaire-based study, 62.5% of physicians replied that they would prescribe boost dose. The most common boost doses that were prescribed included 10 Gy in 5 fractions and 14.4 Gy in 8 fractions. Furthermore, 58.7% of physicians responded that they preferred to not use bolus in their treatments. However, 90% responded that they would use bolus for the patient with positive surgical resection margins (case 5) (Fig. 3).
In terms of target volume delineation, the structures included in the target volume varied significantly between physicians, even within the same clinical scenario (Figs. 4 and 5; Supplementary Fig. S1). In a case where the patient was diagnosed with initial clinical internal mammary node metastasis (case 3), 13/15 physicians included the internal mammary node in the target volume. In a case of the patient who underwent pre-pectoral reconstruction instead of subpectoral reconstruction (case 4), 11/15 physicians included the tissue expander in the target volume. The dose-volume histograms were also analyzed. As for the planning target volume (PTV), it varied widely between physiciansâ plans, even within the same clinical scenario. The median PTV volume was 563.67 mL (range, 278.84 to 1,100.77 mL; standard deviation [SD], 209.05 mL). Similarly, there was a wide difference in the mean lung dose; the median mean lung dose was 13.26 Gy (range, 5.33 to 18.80 Gy; SD, 4.60 Gy). There was also a wide variance in terms of lung V5 and V20; their median values were 43.89 mL (range, 16.35 to 99.45 mL; SD, 26.64 mL), 23.65 mL (range, 6.7 to 34.03 mL; SD, 10.30 mL), respectively (Table 4).
Discussion and ConclusionAccording to the Korean Breast Cancer Society (KBCS) registry, the number of breast reconstruction surgeries has increased almost 3-fold between 2002 and 2013 [12]. In the 2017 KBCS report, the rate of reconstruction after mastectomy was 39.1%, 33.7%, and 9.4% in those in the age-group of <40, 40â59, and â„60 years, respectively [13]. In the present study, approximately one-third of patients who underwent PMRT underwent breast reconstruction and this rate is expected to increase in the future. The primary goal in the treatment of women with breast cancer who undergo reconstruction and PMRT is to minimize the complications without compromising the oncological outcomes. Therefore, understanding the practice patterns is crucial for the communication between the patients and surgeons. To our knowledge, this is the first study to report the practice patterns of PMRT in the setting of breast reconstruction in Korea.
Both RT techniques and breast reconstruction techniques have evolved over time. In the present study, a majority of the patients underwent immediate reconstruction; the rate of one-stage, two-stage, autologous-based, and prosthetic-based reconstruction was 51%, 49%, 23%, and 60.5%, respectively. The selection of the reconstruction material is individualized for each patient based on several patient, anatomical, and disease-specific factors, such as comorbidities, shape and size of the breast, availability of tissue around the breast and other donor sites, and planned adjuvant therapy. However, as presented in Fig. 1, we observed wide inter-hospital variability in the use of breast reconstruction material, which reflected that the hospital where a patient underwent the reconstruction dominantly influenced the decision-making regarding the same. Considering that the thickness of post-mastectomy spared skin flap is one of the major determinants of one-stage immediate reconstruction and the rate of reconstruction complications, the choice of breast reconstruction can also be affected based on whether a patient underwent skin-sparing mastectomy. According to a survey in the United States, implant-based reconstruction was highly utilized in the setting of bilateral mastectomy [14]. Similarly, there have been substantial developments in the use of implant-based techniques and decrease in the use of autologous reconstruction materials.
In the setting of prosthetic reconstruction, 87.9% of patients in the current study underwent partial deflation of the tissue expanders before RT and only 9.3% had full inflation during RT, which was in contrast to the practice patterns in the United States where 75.2% of the respondents specified that they do not routinely deflate the expander before RT [15]. Given that recent retrospective studies from Korea reported that maximal inflation status at the time of RT was significantly associated decreased risk of reconstruction-related complications [16], this issue needs to be discussed with reconstructive surgeons and investigated further in the future.
Interestingly, we found more heterogeneity in the details regarding radiation. Firstly, two-thirds of the patients were treated with conventional fractionation while a few large-volume hospitals preferred hypofractionation RT schedules with various regimens. Data supporting hypofractionation RT following mastectomy are still very limited, especially, when accompanied by breast reconstruction [17]. In 2019, we previously reported that hypofractionation RT (40 Gy in 15 fractions) may mitigate the risk of complications in two-stage prosthetic breast reconstruction [18]. Currently, several randomized trialsâAlliance A221505 (NCT03414970), FABREC (NCT03422003)âare underway to investigate the role of hypofractionation RT in reconstructed breasts. Secondly, the use of boost RT was underutilized in the present cohort (15.6%) in contrast with a US survey in 2014, in which 66.5% of respondents indicated that they would prescribed boost RT [15]. A recent study from Harvard suggests that boost RT was significantly associated with reconstruction-related complications and reconstruction failure and that it does not improve local tumor control [19]; therefore, routine use of boost RT should be avoided and risk-to-benefit assessment is recommended. Bolus was applied in 53.5% of the patients, which is similar to the results of the US survey in which a majority of respondents (52.2%) stated that bolus is used in the setting of tissue expanders [15].
The most interesting finding of the present study is the startling variability in the target delineation and RT plans between physicians as well as clinical scenarios (Fig. 5; Supplementary Fig. S1). In contrast to field-based PMRT techniques, in volume-based RT planning, the variations in the target could significantly influence RT-related toxicities and/or oncological outcomes. In this context, the European Society for radiotherapy and OncologyâAdvisory Committee in Radiation Oncology Practice (ESTROâACROP) presented multidisciplinary consensus-based target volume guidelines in the setting of PMRT after implant-based immediate reconstruction [20,21] that could play an important role in reducing the inter-physician variability.
There are several limitations to this study. First, the current study did not represent the whole population of Korea. Despite the best efforts, 16 institutions participated in this study and only six physicians completed the final submission for the dummy run study. Second, this cross-sectional study only included data of 2 years; therefore, a follow-up study is needed to identify further findings. Third, the data regarding reconstruction in patients who did not receive PMRT was lacking and, hence, the generalization of these findings to all breast reconstruction practices in Korea is limited. Reconstruction complications and their predictors will be discussed in another article.
In conclusion, in Korea, breast reconstruction has become an important consideration in the multidisciplinary management of patients with breast cancer due to the importance of the psychosocial functions of the symmetric breast mound. Our studyâs findings regarding the variability in reconstruction and PMRT details, therefore, provide valuable information to physicians and patients. As the reconstructive and therapeutic options become more sophisticated, this balance will be on the forefront of further cancer treatment. Multidisciplinary collaboration between radiation oncologists, surgical oncologists, plastic surgeons, and medical oncologists is imperative to deliver the best care to our patients. Our multi-center prospective observational study (NCT03523078) is underway to evaluate patient satisfaction and cosmetic outcomes according to breast reconstruction and different type of PMRT.
AcknowledgmentsThis study was supported by the Research Grant of the Korean Foundation for Cancer Research (No. 2017-B-3).
Supplementary MaterialsSupplementary materials can be found via http://doi.org/10.3857/roj.2020.00738
Fig. S1Radiation therapy structures included according to each clinical scenario. (A) Case 1: pT2N (3/12). (B) Case 2: pT3N (7/22) with pathologic axillar level 1 node positive. (C) Case 3: icN3 (internal mammary node positive) â ypT2N (5/15). (D) Case 4: pT2N (5/22) with pre-pectoral reconstruction. (E) Case 5: pT2N (3/16) with positive resection margin. Supplementary A.Answers on a questionnaire regarding the infrastructural information Fig. 1.Reconstruction details. (A) One-stage vs. two-stage reconstruction. (B) Prosthetic vs. autologous reconstruction. (C) Materials used for reconstruction. (D) Inflation status of the tissue expander at the time of radiation therapy. TRAM, transverse rectus abdominis myocutaneous; DIEP, deep inferior epigastric perforator; LD, latissimus dorsi; TUG, transverse upper gracilis; IGAP, inferior gluteal artery perforator; SIEA, superficial inferior epigastric artery; PAP, profunda artery perforator. 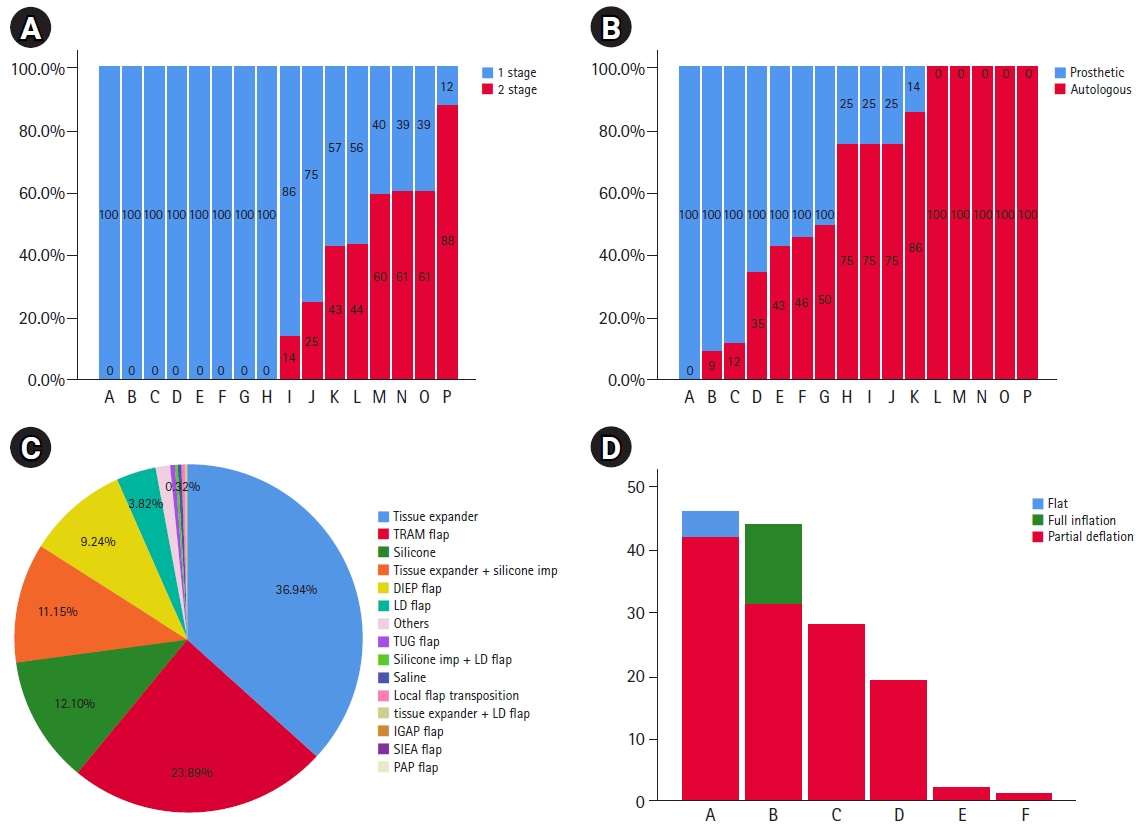
Fig. 4.Structures included in target volume delineation according to different clinical scenarios. AXL, axillary lymph node; SCL, supraclavicular lymph node; IMN, internal mammary node. 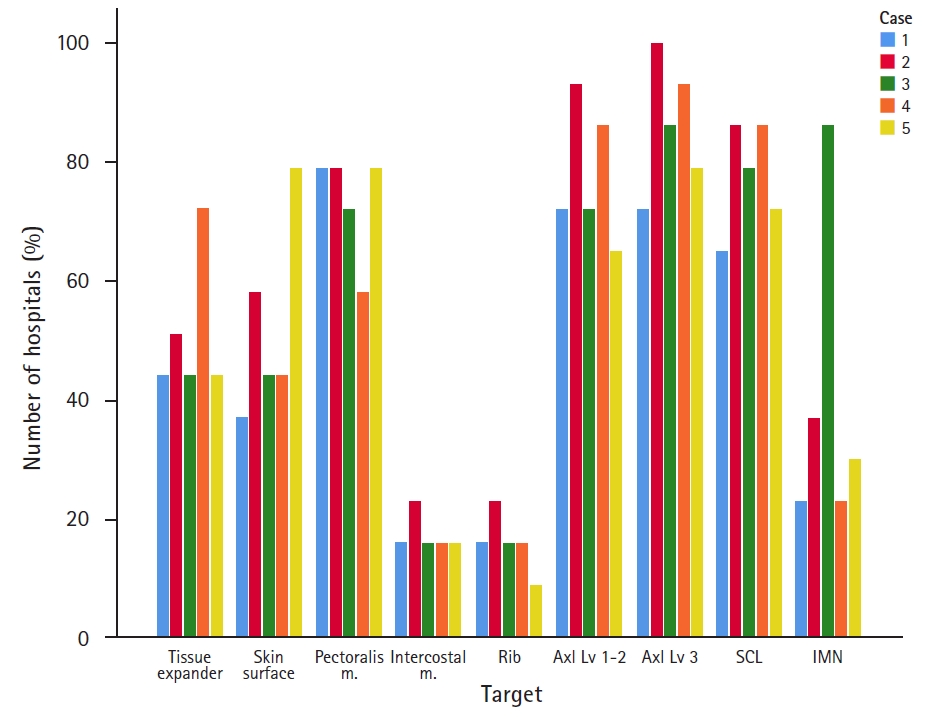
Fig. 5.Sum of all the radiation therapy structures included according to each clinical scenario. (A) Supraclavicular level. (B) Axillary level. (C) Upper reconstructed breast level. (D) Reconstructed breast level. 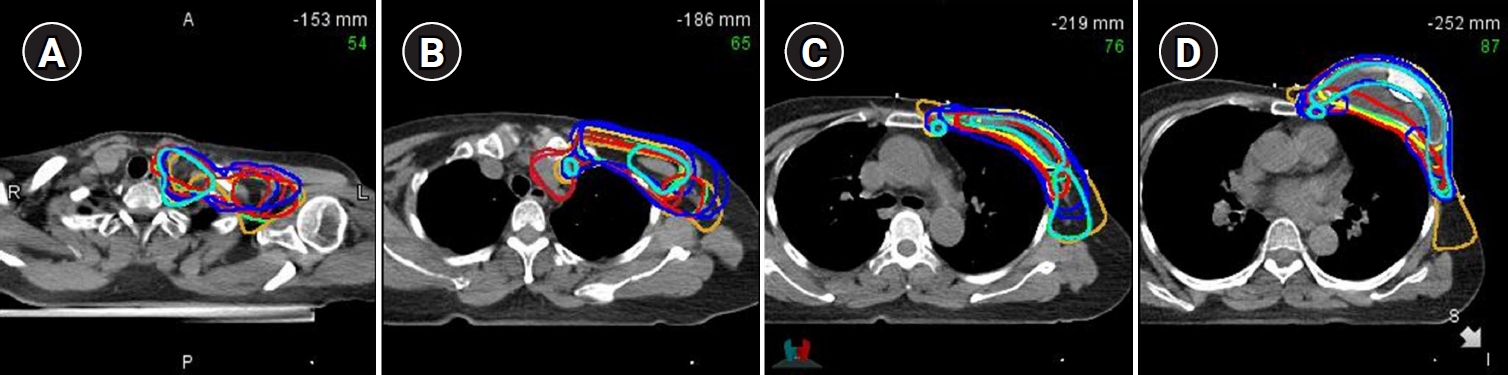
Table 1.Baseline characteristics (n = 314) Table 2.Reconstruction treatments (n = 314) Table 3.Radiation treatments (n = 314) Table 4.Dose volume histograms in the same representative case References1. Panchal H, Matros E. Current trends in postmastectomy breast reconstruction. Plast Reconstr Surg 2017;140(5S):7Sâ13S.
2. Oh C, Winocour SJ, Lemaine V. Latest trends in subpectoral breast reconstruction. Semin Plast Surg 2019;33:224â8.
3. Nelson JA, Allen RJ Jr, Polanco T, et al. Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg 2019;270:473â83.
4. Ho TB, Wood WC, Mspt PD. Breast reconstruction in the setting of postmastectomy radiotherapy: controversies and disparities. Oncology (Williston Park) 2019;33:688845.
5. Ho AY, Hu ZI, Mehrara BJ, Wilkins EG. Radiotherapy in the setting of breast reconstruction: types, techniques, and timing. Lancet Oncol 2017;18:e742âe753.
6. Chawla AK, Kachnic LA, Taghian AG, Niemierko A, Zapton DT, Powell SN. Radiotherapy and breast reconstruction: complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys 2002;54:520â6.
7. Rozen WM, Ashton MW. Radiotherapy and breast reconstruction: oncology, cosmesis and complications. Gland Surg 2012;1:119â27.
8. Thamm OC, Andree C. Immediate versus delayed breast reconstruction: evolving concepts and evidence base. Clin Plast Surg 2018;45:119â27.
9. Xu F, Sun H, Zhang C, et al. Comparison of surgical complication between immediate implant and autologous breast reconstruction after mastectomy: a multicenter study of 426 cases. J Surg Oncol 2018;118:953â8.
10. Lemaine V, Schilz SR, Van Houten HK, Zhu L, Habermann EB, Boughey JC. Autologous breast reconstruction versus implant-based reconstruction: how do long-term costs and health care use compare? Plast Reconstr Surg 2020;145:303â11.
11. Jagsi R, Momoh AO, Qi J, et al. Impact of radiotherapy on complications and patient-reported outcomes after breast reconstruction. J Natl Cancer Inst 2018;110:157â65.
12. Min SY, Kim Z, Hur MH, et al. The basic facts of Korean Breast Cancer in 2013: results of a nationwide survey and breast cancer registry database. J Breast Cancer 2016;19:1â7.
13. Kang SY, Kim YS, Kim Z, et al. Breast cancer statistics in Korea in 2017: data from a breast cancer registry. J Breast Cancer 2020;23:115â28.
14. Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in U.S. breast reconstruction: increasing implant rates. Plast Reconstr Surg 2013;131:15â23.
15. Thomas K, Rahimi A, Spangler A, Anderson J, Garwood D. Radiation practice patterns among United States radiation oncologists for postmastectomy breast reconstruction and oncoplastic breast reduction. Pract Radiat Oncol 2014;4:466â71.
16. Woo KJ, Paik JM, Bang SI, Mun GH, Pyon JK. The impact of expander inflation/deflation status during adjuvant radiotherapy on the complications of immediate two-stage breast reconstruction. Aesthetic Plast Surg 2017;41:551â9.
17. Smith NL, Jethwa KR, Viehman JK, et al. Post-mastectomy intensity modulated proton therapy after immediate breast reconstruction: Initial report of reconstruction outcomes and predictors of complications. Radiother Oncol 2019;140:76â83.
18. Chang JS, Song SY, Oh JH, et al. Influence of radiation dose to reconstructed breast following mastectomy on complication in breast cancer patients undergoing two-stage prosthetic breast reconstruction. Front Oncol 2019;9:243.
19. Naoum GE, Salama L, Ho A, et al. The impact of chest wall boost on reconstruction complications and local control in patients treated for breast cancer. Int J Radiat Oncol Biol Phys 2019;105:155â64.
|
|
||||||||||||||||||||||||||||||||||||||||||||||

 |
 |