 |
 |
AbstractPurposeWe evaluate various approaches to target volume definition and boost delivery in patients with complete response to neoadjuvant systemic therapy (NST) who were treated by radiotherapy without a surgery.
Materials and MethodsA pathological complete response (pCR) was diagnosed in 21 of 27 patients included in “surgery de-escalation” prospective observation study. Clips were placed in the primary tumor volume (PrTV) before NST and during the vacuum aspiration biopsy. Twenty patients with pCR underwent the whole breast irradiation and a boost to the PrTV. High-dose rate brachytherapy (HDRB) was the basic technique for boost delivery. Finally, we identified the value of fused images (computed tomography [CT] before NST with simulation CT), clips and their combination for an accurate boost delivery.
ResultsA complete overlap between PrTV on pre-treatment CT with the localization of the clips on simulation CT was mentioned in 10, partial mismatch in three patients. In 12 of these 13 women, HDRB was successfully used for the boost delivery. In five cases we mentioned a marked discrepancy between the PrTV on fused images and the topography of the clips. In other two women we did not find clips on simulation CT. The fused images in five of these seven patients showed anatomical landmarks (scar, fibrosis) used for identification of the gross tumor volume. In all 20 women with pCR (average follow-up of 16.6 months), there were no locoregional recurrences.
IntroductionIn patients with triple negative and epidermal growth factor receptor 2-positive (HER2+) breast cancer (BC), modern neoadjuvant systemic treatment (NST) is associated with 60%–80% of pathological complete response (pCR) and improved prognosis [1-3]. It seems that eradication of viable tumor cells advocates for a less aggressive locoregional treatment strategy in these exceptional responders to systemic therapy. Some preliminary data indicate that modern methods of functional imaging are accurate in predicting pCR [4]. On the other hand, markers-guided vacuum-assisted biopy (VAB) is proposed as the option of “de-escalated” minimal invasion surgery permitting pathomorphological evaluation of tumor response to NST [5]. In 2019, we started a single center prospective observation study of surgery de-escalation in BC patients with pCR to NST. The combination of instrumental diagnostic procedures with VAB is used in protocoling to identify patients with complete response to systemic therapy. Taking into account that in some studies [6,7] the false negative rate of VAB in pCR diagnosis reaches 15%–25%, we consider that radiotherapy with an obligatory boost to the primary lesion is an important component of our protocol. After launching this study, we recognized several different scenarios that influenced the strategy of boost delivery: in some cases, brachytherapy was substituted for external-beam boost, in others gross tumor volume (GTV) was expanded, or “surrogate markers” (fibrosis) were used for implantation and GTV identification.
The aim of this study was to analyze different approaches to target volume definition and boost delivery in complete responders: clips-based strategy, fusion of primary computed tomography (CT) images with simulation CT and combinations of both methods.
Materials and MethodsThe single center prospective observation study “Refusal of surgical treatment in patients with pCR after NST of triple negative or HER2-positive BC” was initiated in 2019. The primary endpoint of the study is a 3-year ipsilateral local recurrence rate. The secondary endpoint is a 5-year overall and a relapse-free survival. The protocol was approved by the Institute’s Ethics Committee of N.N. Petrov National Cancer Center (No. 1/107, dated 15.08.2019). A written voluntary informed consent was obtained from all patients. Details of this protocol are presented on ClinicalTrials.gov (NCT04293796). Briefly, the inclusion criteria were as follows: women with early (T1-2 N0-1 M0) triple negative or HER2+ BC with lesions not more than 3 cm who received NST according to the protocol. Patients with multicentric disease and women who did not receive the full program of NST and/or indicated radiotherapy, were excluded from the study. All 27 women registered in the study in March 2023 were included in this preliminary analysis. Patients’ characteristics are presented in Table 1. All women included in the trial underwent standard staging with mammography, breast and regional lymph nodes ultrasound with obligatory aspiration biopsy of suspicious lymph nodes. As single photon emission computed tomography-CT (SPECT-CT) with 99mTc-metoxiisobutilisonitril was characterized by high accuracy in diagnosing local extent and lymph node involvement by BC [8], these examinations were used as obligatory for primary staging. Taking into account that in our practice the supine position with the hand behind the head is standard for SPECT-CT examinations of the breasts, it was possible to use CT component of SPECT-CT data for further fusion with simulation CT. Another important component of the study was obligatory clipping of the primary lesion and suspicious/confirmed metastatic lymph nodes before the starting NST.
Details of NST are presented in Table 1. Two–four weeks after the end of neoadjuvant program, all patients underwent mammography, ultrasound, and molecular breast imaging. Subsequent surgical restaging consisted of sentinel lymph node biopsy combined with the excision of clipped suspicious/confirmed metastatic lymph nodes (targeted biopsy) and simultaneous ultrasound-guided VAB with pathomorphologic verification of tumor response to NST. During VAB the primary tumor area was again marked by at least three clips. In patients with residual disease determined as non-complete response in primary tumor and/or axillary lymph nodes, standard surgical treatment with/without adjuvant radiotherapy was initiated according to national guidelines. In women with pCR adjuvant radiotherapy was used as the only adjuvant loco-regional treatment. The whole-breast irradiation (WBI) was performed through tangential fields using the “field-in-field” technique. Initial 15 patients received WBI as 25 fractions of 2 Gy, the rest six patients as 16 fractions of 2.7 Gy. Boost to the primary tumor volume was considered as an obligatory component of adjuvant radiotherapy. As high-dose rate brachytherapy (HDRB) is assumed as a preferred technique for boost delivery, it was performed within 1 week after WBI. Interstitial plastic or steel needles (catheters) were placed using intravenous sedation and anaesthesia. Implantations were performed under CT control following the Paris system geometric recommendation.
Planning boost delivery was performed in accordance with the general principles: GTV, the volume of the tumor that was determined before NST; and clinical target volume (CTV), 10–20 mm area around GTV with an increased risk of subclinical invasion of the tumor. Fortunately, in case of “non-surgical” BC treatment, the shape and volume of the breast were similar before the treatment and at the moment of boost delivery. In accordance with the standard technique of postoperative boost delivery, we proposed that clips placed after VAB could be used as the “cornerstones” for delineation of GTV. The Groupe Européen de Curiethérapie–European Society for Radiotherapy and Oncology (GEC-ESTRO) guidelines recommend using images of the primary lesion obtained before the surgery as an additional tool for GTV and CTV contouring [9]. In the presented study, we fused CT component of primary staging SPECT-CT in the supine position with simulation CT in the supine position with hand above the head performed just before the image-guided HDRB or during simulation for external-beam radiotherapy boost. Taking into account possible differences in the position of the arms and bones, the manual 3-dimensional fusion procedure was primarily based on the contours of the breast and localisation of the sub-mammary fold. Another important point for the fusion was the localisation of the nipple. Sternum and ribs were considered as additional but not obligatory fusion points. After the fusion, we determined the correspondence between the position of the clips and primary tumor volume. If the markers accurately corresponded the primary tumor volume, we considered those cases as complete overlap of the volumes; when markers were partly inside and partly outside the primary tumor volume with the distance to primary tumor contour below 2 cm, we determined those cases as a partial mismatch. All other cases were evaluated as marked discrepancy.
Treatment planning was performed on Oncetra Brachy (Elekta, Stockholm, Sweden) planning system by the automatic and graphical dose optimization. HDRB boost dose was delivered as 7 fractions of 2 Gy in/within 4 days or 3 fractions of 4 Gy in/within 3 days. The minimal interval between fractions was 6 hours, maximal 20 hours. External-beam radiotherapy was considered as an alternative “boost” technique in women who refused HDRB or when it was considered suboptimal, for example, when the tumor was localized close to the skin.
ResultsFrom February 2020 to March 2023, 27 consecutive patients (mean age, 48.9 years; range, 35 to 68 years) were included in the study: 24 women obtained clinical complete response (cCR) and 21 of them obtained pCR to the NST (Table 2). The follow-up period ranged from 9 to 26 months (average of 16.6 months). During the follow-up, there were no cases of local and/or regional failure.
After the WBI, 20 of 21 women with pCR finished the treatment according to the protocol and received boost to the primary tumor volume: in 18 cases by HDRB and in the remaining 2 with external-beam radiotherapy. One woman was irradiated in the regional hospital and was excluded from the study. In the remaining 20 patients, pretreatment SPECT-CT (CT component) was fused with simulation CT (in the cases of HDRB before needle insertion).
Data analysis following the fusion demonstrates a complete overlap of primary tumor volumes on SPECT-CT images with the localization of the clips on simulation CT (Fig. 1A, 1B) in 10 of 20 evaluated patients. We mentioned that even after very gentle needle insertion, dramatic changes in breast shape occurred in most of the cases, and accurate fusion of pre-treatment SPECT-CT with post-implantation planning CT was very difficult or impossible (Fig. 2). For this reason, in post-implantation planning CT, we used clips as the guide for GTV contouring. In one woman of that group, we performed the electron boost because the primary tumor volume on fused images and clips was located close to the skin.
A partial mismatch of the tumor volume on staging SPECT-CT with the position of the clips on simulation CT was mentioned in three cases (Fig. 3). In these patients, final planning GTV (GTVfin) was created as the sum of the GTVfus obtained after the fusion of pre-treatment SPECT-CT with planning CT and GTVclips contoured according to the localization of the clips. From our experience both volumes can be used on planning CT after the needle insertion, so it is the reason for choosing HDRB as the preferred method of boost delivery in these patients too.
The third situation is characterised by a marked discrepancy in the localization of primary lesion in fused images and topography of the clips placed after VAB (Fig. 4). This scenario was mentioned in five observations. The migration of the clips can be considered the most probable explanation of these discrepancies; in addition, technical defects during the clip placement can cause these inaccuracies. Optimal technique of boost delivery and GTV delineation was chosen according to the following algorithm: in those three cases when it was possible (after fusion of SPECT-CT with pre-implantation CT) to identify anatomical landmarks for subsequent brachytherapy planning (the scar and fibrosis in the area of the primary lesion (Fig. 5), HDRB can be considered as an acceptable method for boost delivery. In these cases, the identified anatomical landmarks were used on post-implantation CT for contouring of the GTV. On the contrary, when we failed to find anatomical landmarks for identification of the GTV after the needle insertion in one woman, she was considered for external-beam boost with GTVfin identical to GTVfus (Fig. 5).
In one observation the differences in the topography of GTVclips and GTVfus were pronounced (without overlap of the volumes) and unclear. In that case, we used external-beam radiotherapy as the preferable technique for boost delivery and delineated boost GTVfin as the sum of GTVfus and GTVclips
In the remaining two women we failed to find the clips but both patients had extensive focal fibrotic areas localised directly in the area of primary tumor volume in the fused images. In both cases, we performed “fibrosis-guided” HDRB boost.
Discussion and ConclusionIn the presented study group, modern NST demonstrated high (77.8%) rate of pCR comparable with the data of some other studies [1-3]. This indicates that many recent patients with triple negative and Her2+ BC can be good candidates for the surgery de-escalation. On the other hand, our recent unpublished research of 97 patients with residual BC after NST treated with a standard surgery with postoperative irradiation indicates that 5-year rates of locoregional relapses were even higher than distant failure: 20% versus 19% in triple-negative, and 8% versus 6% in HER2+ BC. This leads us to the following: the adjuvant radiotherapy with obligatory boost to the primary tumor volume must be considered as an important part of protocols with surgery de-escalation. The choice of HDRB as the basic method of boost delivery has several reasons. From one point of view, dosimetric studies demonstrate that brachytherapy boost compared to external-beam techniques is characterized by significantly lower doses to the organs-at-risk [10]; first of all, by significant reduction (2–10 times) of the ipsilateral breast irradiated volume [11]. In addition, it is well known that HDRB technique is characterized by the measurable inhomogeneity of dose distribution. According to GEC-ESTRO recommendation, in patients with BC HDRB the boost non-uniformity index must be kept below 0.35 in order to preserve good cosmetic results [9]. This means that up to one-third of boosting tumor volume would receive 150% and more of the prescribed dose and probably because of this feature the brachytherapy boost is associated with the highest local control [12,13]. In particular, Poortmans et al. [12] in the largest prospective multicenter randomized boost study reported only 2.3% recurrence rate after brachytherapy boost and nonsignificant but substantial increase in local recurrence rate after electron or photon boosts (4.7% and 4.0%, respectively). Of special value for our decision was the study of Guinot et al. [13] stating that 248 BC patients with close or positive resection margins demonstrated that even in this unfavorable clinical situation HDRB can successfully substitute re-resection with free margins: 86.9%–96.2% 10-year local tumor control can be reached with 3 × 4.4 Gy HDRB boost.
Placement of the clips is a simple and perfectly validated tool for accurate identification of the primary tumor volume used for boost delivery. Unfortunately, VAB performed for a pathologic verification of tumor response took away those clips together with the tumor sample. As was shown in our study, the secondary clipping of the VAB area can successfully navigate the delivery of the boost to the primary tumor volume in many (65%) but not in all cases. In some patients (35%) the displacement of the clips can be corrected by anatomical landmarks of the primary tumor volume. In most difficult situations when clip displacement is associated with the absence of anatomical landmarks of primary tumor, the best solution for boost delivery seems to be external-beam radiotherapy with the use of fused images for GTV contouring. The diversity of clinical situations indicates that the “verification” fusion of the primary CT with the simulation CT is a very useful tool for identification of the optimal strategy for boost delivery.
Now it is possible to mention that the strategy of surgery de-escalation is only making its first steps: from the early publications [14-16] to the recent reports [5,17] the opportunities of nonsurgical treatment of BC were discussed with cautions. Mature results of few ongoing studies would be probably able to change this situation.
From our point of view, the attempts for eliminating VAB can be a very interesting and promising opportunity for further development of this strategy that would convert minimal invasive treatment to non-invasive protocols. A low diagnostic accuracy of modern diagnostic modalities (positron emission tomography-CT, magnetic resonance imaging, ultrasound, mammography) in predicting pCR is considered the main obstacle on the way to refuse invasive diagnostic procedures such as VAB [18]. On the other hand, it was already demonstrated that scintimammography performed in the middle of NST could identify (with moderate sensitivity but very high specificity patients (94%) who could reach pCR after the end of NST [19]. It seems that in these patients, VAB particularly can be safely omitted, and women can be treated with a “no surgery” approach. Even if we assume that the risk to overestimate the response to NST in these cases is slightly higher than after VAB, the adjuvant radiotherapy with local boost would probably be able to control this misdiagnosed “pCR.”
In conclusion, we would like to propose several recommendations for the radiotherapy part of surgery de-escalation protocols.
Similarities in the shape and volume of the breast along the whole treatment time in patients included in the protocol of BC treatment with surgical de-escalation permit an effective utilization of pre-NST CT and simulation CT fusion before the boost delivery. Fusion enables visualization of the primary tumor volume and verification of correct/incorrect localization of clips that mark the primary tumor volume.
Brachytherapy boost can be performed in women with correct clip placement and in cases when primary tumor volume can be correctly determined with the help of anatomical landmarks. In the remaining patients, boost delivery with external-beam radiotherapy seems more accurate and effective.
NotesStatement of Ethics The study was approved by the Institute’s Ethics Committee (No. 1/107, dated 15.08.2019). A written voluntary informed consent was obtained from all patients. Author Contributions Conceptualization, Novikov SN, Krivorotko P, Kanaev S. Investigation and methodology, Novikov SN, Krivorotko P, Bryantseva Z, Akulova I, Krzhivitskiy P. Data curation, Emelyanov A, Krzhivitskiy P, V, Ponomareva O. Writing of the original draft, Novikov SN, Bryantseva Z, Emelyanov A, Kanaev S. Writing of the review and editing, Novikov SN, Krivorotko P, Bryantseva Z, Akulova I, Emelyanov A, Mortada V, Ponomareva O, Krzhivitskiy P, Kanaev S. Fig. 1.Complete overlap of primary tumor volume and clips placed during vacuum aspirated biopsy. (A) CT image from staging SPECT-CT with 99mTc-methoxyisobutylisonitrile. Primary tumor volume clearly identified and contoured with the red line. (B) Fusion of the staging CT with simulation CT performed before needle insertion. Primary tumor volume contoured with the red line, clips perfectly correspond to the primary tumor volume. CT, computed tomography; SPECT, single photon emission computed tomography. 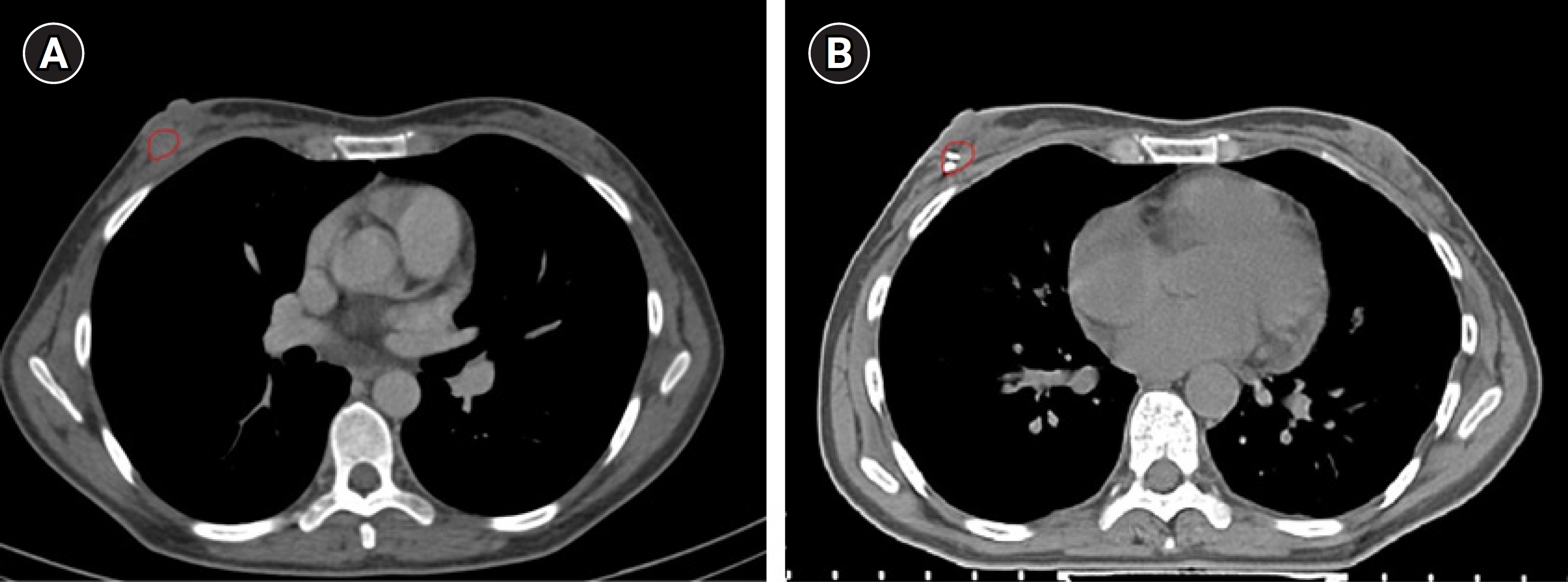
Fig. 2.Prominent differences in the breast shape and volume on the computed tomography images obtained before and after the implantation of the needles for brachytherapy. 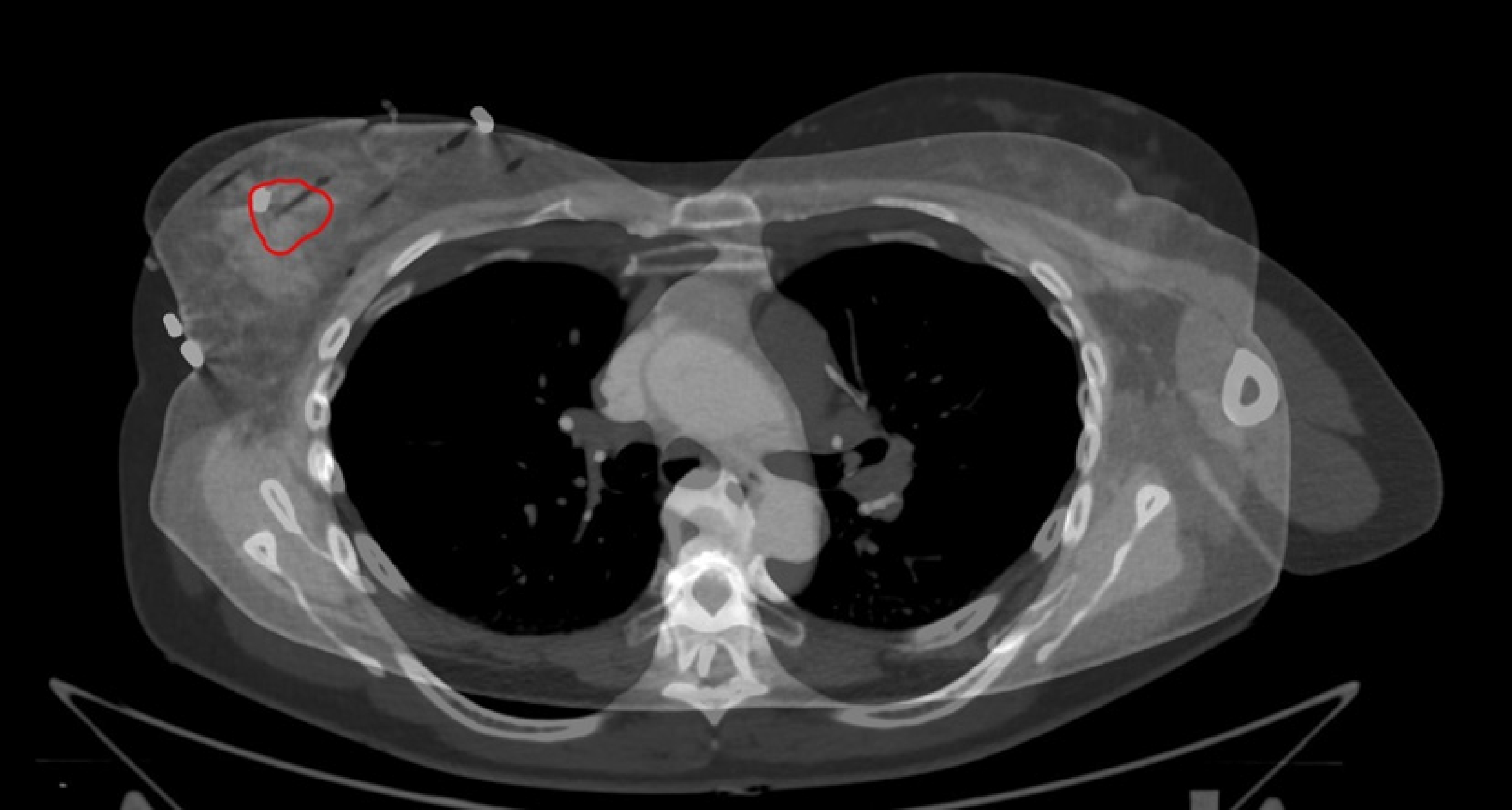
Fig. 3.Fused images of CT performed before starting treatment (from staging SPECT-CT) and simulation CT before boost delivery. Example of partial mismatch between the tumor contours on staging CT (red) with the position of the clips on simulation CT (white arrow). Final GTV (yellow) created as the sum of the GTV delineated after fusion (red) and expansion of this volume to cover clips placed during vacuum aspirated biopsy. CT, computed tomography; SPECT, single photon emission computed tomography; GTV, gross tumor volume. 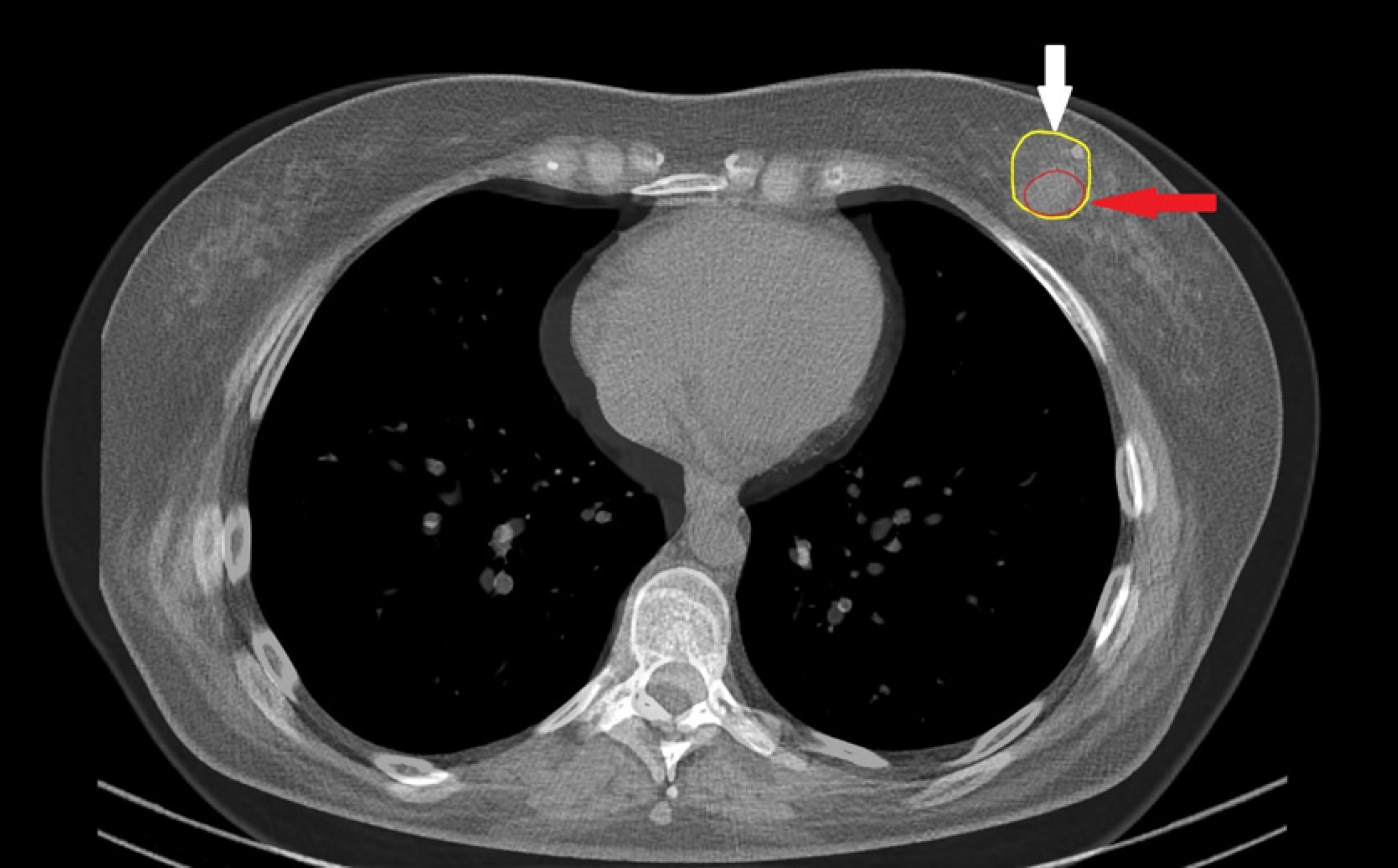
Fig. 4.Fused images of CT performed before starting treatment (from staging SPECT-CT) and simulation CT. Major mismatch between primary tumor volume (red) and localization of the clips (white arrow). In this case, boost to the primary tumor area was performed by external-beam radiotherapy, gross tumor volume contoured on fused images according to the localization of the primary lesion on SPECT-CT. CT, computed tomography; SPECT, single photon emission computed tomography. 
Fig. 5.Focal fibrosis that helps identifying primary tumor volume. (A) CT image from staging SPECT-CT with 99mTc-methoxyisobutylisonitrile. Primary tumor volume clearly identified and contoured with the red line. (B) Fusion of the staging CT with simulation CT performed before needle insertion. On fused images, focal fibrosis (white arrow) perfectly corresponds to the localization of the primary tumor volume (red contour). This anatomical landmark guided needle insertion was used for contouring gross tumor volume for boost delivery. CT, computed tomography; SPECT, single photon emission computed tomography. 
Table 1.Baseline patient, tumor, and treatment characteristics Values are presented as median (range) or number (%). HER2+, epidermal growth factor receptor 2 positive; AC+T, doxorubicin and cyclophosphamide followed by paclitaxel; AC+TC, doxorubicin and cyclophosphamide followed by paclitaxel and carboplatin; DCHP, docetaxel, carboplatin, trastuzumab, and pertuzumab; АС+DHP, doxorubicin and cyclophosphamide followed by docetaxel, trastuzumab, and pertuzumab. Table 2.Outcome data in patients included in the study
References1. Santonja A, Sanchez-Munoz A, Lluch A, et al. Triple negative breast cancer subtypes and pathologic complete response rate to neoadjuvant chemotherapy. Oncotarget 2018;9:26406–16.
2. Gianni L, Pienkowski T, Im YH, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. Lancet Oncol 2012;13:25–32.
3. Shepherd JH, Ballman K, Polley MC, et al. CALGB 40603 (Alliance): long-term outcomes and genomic correlates of response and survival after neoadjuvant chemotherapy with or without carboplatin and bevacizumab in triple-negative breast cancer. J Clin Oncol 2022;40:1323–34.
4. Guo C, Zhang C, Liu J, Tong L, Huang G. Is Tc-99m sestamibi scintimammography useful in the prediction of neoadjuvant chemotherapy responses in breast cancer? A systematic review and meta-analysis. Nucl Med Commun 2016;37:675–88.
5. Kuerer HM, Smith BD, Krishnamurthy S, et al. Eliminating breast surgery for invasive breast cancer in exceptional responders to neoadjuvant systemic therapy: a multicentre, single-arm, phase 2 trial. Lancet Oncol 2022;23:1517–24.
6. Heil J, Schaefgen B, Sinn P, et al. Can a pathological complete response of breast cancer after neoadjuvant chemotherapy be diagnosed by minimal invasive biopsy? Eur J Cancer 2016;69:142–50.
7. van Loevezijn AA, van der Noordaa ME, van Werkhoven ED, et al. Minimally invasive complete response assessment of the breast after neoadjuvant systemic therapy for early breast cancer (MICRA trial): interim analysis of a multicenter observational cohort study. Ann Surg Oncol 2021;28:3243–53.
8. Krzhivitskii PI, Novikov SN, Kanaev SV, et al. The use of single-photon emission computed tomography-computed tomography in detecting multiple metastatic lymph nodes in patients with breast cancer. Nucl Med Commun 2019;40:169–74.
9. Strnad V, Major T, Polgar C, et al. ESTRO-ACROP guideline: interstitial multi-catheter breast brachytherapy as accelerated partial breast irradiation alone or as boost: GEC-ESTRO Breast Cancer Working Group practical recommendations. Radiother Oncol 2018;128:411–20.
10. Terheyden MM, Melchert C, Kovacs G. External beam boost versus interstitial high-dose-rate brachytherapy boost in the adjuvant radiotherapy following breast-conserving therapy in early-stage breast cancer: a dosimetric comparison. J Contemp Brachytherapy 2016;8:294–300.
11. Akulova IA, Bryantseva ZV, Novikov SN, Kanaev SV, Melnik JS. 3-D conformal external beam radiotherapy and interstitial HDR brachytherapy for adjuvant breast irradiation: dosimetric comparison. Med Phys 2020;85:67–74.
12. Poortmans P, Bartelink H, Horiot JC, et al. The influence of the boost technique on local control in breast conserving treatment in the EORTC 'boost versus no boost' randomised trial. Radiother Oncol 2004;72:25–33.
13. Guinot JL, Tortajada MI, Santos MA, et al. Can invasive breast carcinoma with close or positive margins be managed without a new surgery? Breast J 2018;24:1024–7.
14. De Lena M, Varini M, Zucali R, et al. Multimodal treatment for locally advanced breast cancer: result of chemotherapy-radiotherapy versus chemotherapy-surgery. Cancer Clin Trials 1981;4:229–36.
15. Ring A, Webb A, Ashley S, et al. Is surgery necessary after complete clinical remission following neoadjuvant chemotherapy for early breast cancer? J Clin Oncol 2003;21:4540–5.
16. Perloff M, Lesnick GJ, Korzun A, et al. Combination chemotherapy with mastectomy or radiotherapy for stage III breast carcinoma: a Cancer and Leukemia Group B study. J Clin Oncol 1988;6:261–9.
17. Kuerer HM, Rauch GM, Krishnamurthy S, et al. A clinical feasibility trial for identification of exceptional responders in whom breast cancer surgery can be eliminated following neoadjuvant systemic therapy. Ann Surg 2018;267:946–51.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |