 |
 |
AbstractPurposeTo evaluate set-up error for head and neck cancer (HNC) patients according to each neck lymph node (LN) level. And clinical factors affecting set-up error were analyzed.
Materials and MethodsReference points (RP1, RP2, RP3, and RP4) representing neck LN levels I to IV were designated. These RP were contoured on simulation computed tomography (CT) and cone-beam CT of 89 HNC patients with the same standard. After image registration was performed, movement of each RP was measured. Univariable logistic regression analyses were performed to analyze clinical factors related to measured movements.
ResultsThe mean value of deviation of all axes was 1.6 mm, 1.3 mm, 1.8 mm, and 1.5 mm for RP1, RP2, RP3, and RP4, respectively. Deviation was over 3 mm in 24 patients. Movement of more than 3 mm was observed only in RP1 and RP3. In RP1, it was related to bite block use. Movement exceeding 3 mm was most frequently observed in RP3. Primary tumor and metastatic LN volume change were clinical factors related to the RP3 movement.
ConclusionPlanning target volume margin of 4 mm for neck LN level I, 3 mm for neck LN level II, 5 mm for neck LN level III, and 3 mm for neck LN level IV was required to include all movements of each LN level. In patients using bite block, changes in primary tumor volume, and metastatic LN volume were related to significant movement.
IntroductionHead and neck cancer (HNC) is the seventh most common cancer worldwide. Its incidence is increasing, showing more than 660,000 new cases each year [1]. Radiotherapy (RT) is one of the main treatment options for HNC [2]. Intensity-modulated RT (IMRT) is widely used in HNC to improve oncologic outcomes, reduce RT-related toxicities, and even enable re-irradiation [3]. IMRT is a highly sophisticated RT technique that can deliver a high radiation dose to the target volume while minimizing radiation exposure to nearby organ-at-risk. Paradoxically, the excessive sophistication of this technique makes it more sensitive to errors, which can lead to an inaccurate treatment. Set-up error is among the most significant errors. It is defined as any deviation of the target position during treatment compared to the reference position in the planning computed tomography (CT) scan [4]. Therefore, the use of various image-guided RT (IGRT) techniques and the application of an appropriate planning target volume (PTV) margin are essential for an accurate IMRT.
The PTV is a geometric volume defined to secure the dose delivery to the clinical target volume (CTV) by reflecting set-up and mechanical uncertainties [5]. The HNC CTV is often large from the skull base to the clavicle, including the regional lymphatic chain. If the target is large, the set-up error of the center and the edge of the target might be different. Nevertheless, contouring guidelines related to HNC do not recommend the PTV margin with detailed distinction [6]. The aim of this study was to prove the necessity of subdividing the PTV margin in HNC. Target deviation between planning CT and cone-beam CT (CBCT) was recorded for each neck lymph node (LN) level and clinical factors affecting its deviation were analyzed.
Materials and Methods1. Patient selection and data collectionPatients who underwent curative-intent IMRT for locally advanced HNC from January 2017 to December 2021 at Gyeongsang National University Changwon Hospital were selected for this retrospective analysis. Locally advanced stage was defined as clinical stage III to IVB based on the 8th edition of the American Joint Committee on Cancer [7] except that nasopharyngeal cancer was defined as a locally advanced stage from stage II to stage IVA. Among those with HNC, patients whose primary tumor site was skin, eye, orbit, ear, lip, thyroid, or unknown primary were excluded. Patients with a history of surgery or RT that could cause structural changes in the head and neck or who could not obtain sufficient images to measure target movement due to failure to complete planned RT were excluded from the analysis. This study was approved by the Institutional Review Board of Gyeongsang National University Changwon Hospital (No. 2023-04-005).
Medical records and treatment records (ARIA record and verification system; Varian Medical Systems, Palo Alto, CA, USA) were reviewed. Age, sex, primary tumor location, stage group, contralateral LN metastasis, PTV volume, primary tumor volume change, metastatic LN volume change, body weight change, number of CBCT scans, bite block, and chemotherapy were recorded. The primary tumor location was categorized into three parts: nose, mouth, and neck. The nose part consisted of the nasopharynx (NPX), nasal cavity, and paranasal sinus. The mouth part consisted of the oral cavity, oropharynx, and salivary gland. The neck part consisted of the hypopharynx and larynx. Primary tumor and metastatic LN volume changes were defined as changes between planning CT and re-simulation CT. Body weight change was defined as the difference between the weight measured at the time of diagnosis of HNC and the weight measured within 1 month after RT.
2. Simulation, treatment planning, and set-up proceduresAll patients were immobilized by Type-S Head & Neck, Shoulder Thermoplastic mask (CIVCO, Kalona, IA, USA). Bite block (Sejong Medical, Paju, Korea) was additionally used in the nose and mouth parts of patients. After immobilization, CT simulation with a 3-mm slice thickness was performed using a Brilliance CT Big Bore (Philips Medical Systems, Amsterdam, Netherlands). Scanned CT images were imported into an Eclipse treatment planning system Version 13.7 (Varian Medical Systems). A radiation oncologist delineated the target and normal structure. IMRT was performed using a Varian TrueBeam 2.0 (Varian Medical Systems) with a prescribed total dose of 6,000вҖ“7,200 cGy in 25вҖ“35 fractions.
All patients received the conventional laser set-up procedure using set-up fiducial lines marked on the immobilization mask. After that, CBCT images were periodically obtained once a week for image guidance set-up procedure. Image registration was performed with an automatic algorithm applying a region-of-interest containing the PTV and, if necessary, re-positioned by six-dimensional CBCT guidance. Final set-up corrections were confirmed by a radiation oncologist and manually adjusted when necessary, focusing more on the primary tumor site. Quality assurance procedures for CBCT images and geometrical accuracy analysis were performed monthly to ensure accuracy. During the set-up process, if an error was over 5 mm in any axis, the simulation CT was re-scanned and re-planned. Except for this reason, re-simulation CT was planned after 4,400вҖ“5,000 cGy irradiation due to tumor shrinkage or patient weight loss.
3. Measurement of deviation of neck LN level and statistical analysisNeck LNs were divided into 10 levels based on anatomical configuration and drainage patterns [8]. Among head and neck structures, seven reference points (RP) representing each neck LN level were determined based on the first cervical vertebra, mandible, hyoid bone, manubrium, and sternocleidomastoid muscle, which were clearly distinguished in CBCT (Table 1, Fig. 1). Seven RP were named level I (RP1), and left and right level II (RP2), III (RP3), and IV (RP4), respectively. These RP were consistently drawn on simulation CT and CBCT images. Simulation CT and each CBCT performed image registration using an automatic algorithm, focusing on the PTV and primary tumor site on the same basis as in the treatment. The magnitude of deviation of each RP was recorded with three translational axesвҖ”anterior-posterior (AP), left-to-right (LR), and superior-to-inferior (SI). The overall radial movement was computed as
Results1. Patient characteristicsA total of 89 patients were included in this study. Patient characteristics are summarized in Table 2. Seventy-two patients (80.9%) were male. The median age of all patients at the time of RT was 65 years (range, 33 to 93 years). Numbers of patients with primary tumor location being the nose part, mouth part, and neck part were 16 (18.0%), 33 (37.1%), and 40 (44.9%), respectively. Regarding the stage group, except for NPX, numbers of patients with stage III, IVA, and IVB were 20 (25.6%), 46 (51.7%), and 12 (13.4%), respectively. All patients had LN metastasis and 29 (32.6%) had contralateral LN metastasis. Concurrent chemotherapy was administered to 76 patients (85.4%). Twenty-four patients (27%) used a bite block for immobilization. The CBCT was scanned 606 times, averaging 6.8 times per patient. The median value of the initial PTV volume was 429.3 cm3 (range, 175.8 to 658.8 cm3). Median values of changes in primary tumor volume, metastatic LN volume, and body weight were 19.5% (range, 0% to 76.0%), 29.0% (range, 0% to 87.7%), and 6.0 kg (range, 3.0 to 13.0 kg), respectively.
2. Magnitude of deviation of each reference pointSeven RP represented neck LN levels I, II, III, and IV. A total of 606 CBCT images were compared with simulation CT images. Because the difference between the left and right deviation of each RP was slight, the left and right values were integrated and divided into only RP1, RP2, RP3, and RP4 in the presentation and analysis of the results. Deviation of each RP was recorded in three translational axes and the overall radial movement was calculated. Table 3 and Figs. 2вҖ“5 show the effective magnitude of deviation of each RP. Movement values of all translational axes did not exceed 5 mm. For RP1, the magnitude of deviation exceeded 3 mm in the AP direction in 5 patients (5.6%) and the SI direction in 5 patients (5.6%). RP3 deviations exceeded 3 mm in the LR direction in 1 patient (1.1%) and the SI direction in 21 patients (23.6%). Deviation of more than 3 mm in one or more axial directions was observed in 24 patients (27.0%) regardless of the RP. Regarding radial movement, more than 5 mm was observed in 1 patient (1.1%) in RP1 and 3 patients (3.4%) in RP3. Radial movement of more than 3 mm was observed in 28 patients (31.5%) in RP1, 1 patient (1.1%) in RP2, 50 patients (56.2%) in RP3, and 27 patients (30.3%) in RP4.
3. Factors affecting deviationsA case in which the overall radial movement of each RP was more than 3 mm was defined as an event and related clinical factors were statistically analyzed. RP2, which had a relatively small movement and an event that occurred in only one patient, was excluded from the analysis. Results are summarized in Table 4. Events in RP1 occurred in all patients (100%) who used a bite block. Another factor associated with events in RP1 was primary tumor location (p = 0.002). Significantly fewer RP1 events occurred when the primary tumor location was the neck part. Events in RP3 occurred in all patients (100%) with sufficiently metastatic LN volume change. In addition, statistically significant differences were shown in primary tumor volume change (p = 0.001). RP4 events occurred significantly more in patients with large body weight changes (p = 0.046).
Discussion and ConclusionIt is important to set an appropriate PTV margin because if the PTV margin is too large or too small, unnecessary radiation exposure increases or a sufficient dose is not irradiated to the CTV. Strbac et al. [10] have obtained 632 electronic portal images from 35 HNC patients undergoing RT and found that a PTV margin of at least 6 mm is necessary for CTV to receive a sufficient prescribed dose. Mesko et al. [11] have performed stereotactic ablative RT on 79 patients with recurrent and/or previously irradiated HNC and measured set-up errors according to the treatment site (skull base, neck/parotid, and mucosal). In their study, patients were immobilized at a relatively high level of quality using a cushion, thermoplastic mask, and bite block, and set-up error correction was performed using both ExacTrac X-ray (BrainLAB AG, Munich, Germany) and CBCT. They found that the appropriate PTV margin differed depending on the treatment site, 1.5вҖ“2 mm for the skull base and 2вҖ“2.5 mm for the neck and mucosal area. Based on these previous studies, the PTV margin can be different even if the same head and neck area is treated depending on the institution policy, immobilized device, and IGRT system. Even the margin can differ depending on treatment site. In the present study, patient was immobilized using a thermoplastic mask and bite block. The set-up error was corrected by taking CBCT after laser line set-up. Movements of RP averaged 1.6 mm (range, 0.4 to 4.6 mm). No one had movement over 5 mm. In 24 patients (27.0%), the movement was over 3 mm. Movement of more than 3 mm in any axes was observed only in RP1 and RP3.
Neck LN level I refers to the area combined with submental and submandibular space. Since it is a LN area attached to the inner side of the mandible, movement of the mandible can cause movement of neck LN level I. Therefore, oral fixation has been an essential issue for accurate RT. Various oral devices have been widely used. A bite block, one of the oral fixation devices, can be used to restrict movement of oral tongue or to reduce radiation exposure to adjacent normal tissues such as the salivary gland, mandible, upper gingiva, and hard plate [12]. However, applying bite blocks can have limited reproducibility due to certain medical conditions such as trismus, pain from mucositis, severe gag reflex, and discomfort from holding a bite block, resulting in unexpected target movement [13]. This study observed a statistically significant radial movement of RP1 exceeding 3 mm in patients who used a bite block or whose primary tumor location was the nose or mouth part where the bite block was mainly used. However, because bite block was used in most patients whose primary tumor location was in the nose or mouth part, each factor has the limitation of being a confounding variable for the movement of RP1. Nevertheless, RP1 movement over 3 mm was evident in the AP and SI directions, not the LR. Through this, it can be inferred that the movement of neck LN level I is due to the difference in oral opening caused by variation in bite block application. These results suggest that considering an additional PTV margin for neck LN level I is appropriate when applying a bite block with ongoing development of patient-specific intra-oral devices.
Neck LN level II refers to the upper third of the jugular chain area. It extends from the skull base to the inferior border of the hyoid bone. Several studies have shown that neck LN level II, closer to the base of the skull, has the slightest movement [11,14]. These studies suggest that this area is relatively close to the central axis. Thus, small movements are less amplified and better aligned by the inherently rigid cranial bones with less internal organ movement. Likewise, RP2 had a minor movement in this study compared to other RP, with an average of 1.3 mm in all axes. Only 1.1% had an overall radial movement exceeding 3 mm, suggesting that neck LN level II was fixed the most stably.
Neck LN level III refers to the middle internal jugular chain area between the hyoid superiorly and a horizontal plane defined by the inferior border of the cricoid cartilage. In this study, the movement of the RP exceeding 3 mm was measured the most in RP3 and the movement in the SI direction was particularly prominent. The reason might be due to movement of the hyoid bone, the standard for neck LN level contouring. It is already well known that the hyoid bone moves during a normal swallowing process [15,16]. Radiological and surgical classification of the neck LN level is beneficial in making treatment decisions, comparing treatment results, and communicating with medical staff [17]. However, in the field of RT where fractional treatment is commonly performed, using a moving structure like a hyoid bone as a criterion for distinguishing neck LN levels is likely to impede reproducibility. Thus, it might be necessary to make another neck LN level classification. Factors influencing the radial movement of RP3 were volume change of the primary tumor and metastatic LN. It might be difficult to predict the degree of change in the target volume before treatment. However, if the target has radiosensitive histology, it is necessary to closely observe volume change and perform immediate adaptive RT.
Neck LN level IV refers to the lower third of the jugular chain area. It extends from the inferior border of the cricoid cartilage to the clavicle. This study observed no movement beyond 3 mm in RP4 on any axis. In radial movements that integrated all axes, movements greater than 3 mm were observed, which were correlated with changes in patient's body weight. HNC patients often experience significant weight loss due to inadequate nutrient intake. It is known that such weight loss not only affects the patient's survival, but also leads to inaccurate radiation dose distribution [18]. In patients who are expected to lose weight, it is necessary to appropriately add the PTV margin of neck LN level IV or perform rapid adaptive RT through close monitoring.
The limitation of this study was that the designated RP could not accurately represent each neck LN level. Because it was necessary to define RP that could be clearly distinguished even at the low resolution of CBCT, bone or large muscle became the standard. Because these structures are relatively fixed, movement at each LN level due to clinical factors may have been underestimated. Moreover, set-up errors might vary depending on simulation, immobilization, set-up alignment, image registration, and IGRT system for each hospital policy. Therefore, it is difficult to recommend a PTV margin with an exact value for each neck LN level. Nevertheless, this study is clinically significant because it shows that set-up error differs according to neck LN level and reports clinical factors that could affect the set-up error.
In this study, PTV margins of 4 mm for neck LN level I, 3 mm for neck LN level II, 5 mm for neck LN level III, and 3 mm for neck LN level IV were required to include all movements of each LN level that occurred. Neck LN level II had a minor movement. Neck LN level IV increased the movement according to the patient's weight change. However, no movement exceeding 3 mm was observed. In neck LN level I, movements exceeding 3 mm in AP and SI directions were observed in some patients related to bite block use. Movement exceeding 3 mm was most frequently observed in neck LN level III. Primary tumor and metastatic LN volume change were relevant clinical factors. However, since most neck LN level III movements were biased toward the SI direction, the leading cause might be vertical movement of the hyoid bone during swallowing. Therefore, in patients using bite block, an additional PTV margin for neck LN level I should be considered. If changes in primary tumor volume, metastatic LN volume, and body weight are prominent, rapid adaptive RT is needed. In addition, if a highly mobile structure such as the hyoid bone is used as a standard for classifying the level of neck LN, the range may continue to change during RT, so it is necessary that a new standard for classifying the level of neck LN.
NotesStatement of Ethics This study was a retrospective and informed consent was waived by the Institutional Review Board of Gyeongsang National University Changwon Hospital (No. 2023-04-005), and this study was performed by relevant guidelines and regulations. Author Contributions Conception and design of the study: Choi HS, Jeong BK, and Kang KM. Acquisition of data: Jeong H, Ha IB, and Choi B. Analysis and interpretation of the data: Choi HS, and Kang KM. Writing and revision of the manuscript: Choi HS, and Kang KM. All authors read and approved the final manuscript. Fig.В 1.Seven reference points representing each neck lymph node (LN) level: (A) anterior-posterior view and (B) lateral view. Reference points are shown in red; neck LN level I, green; neck LN level II, white; neck LN level III, blue; and neck LN level IV, yellow. 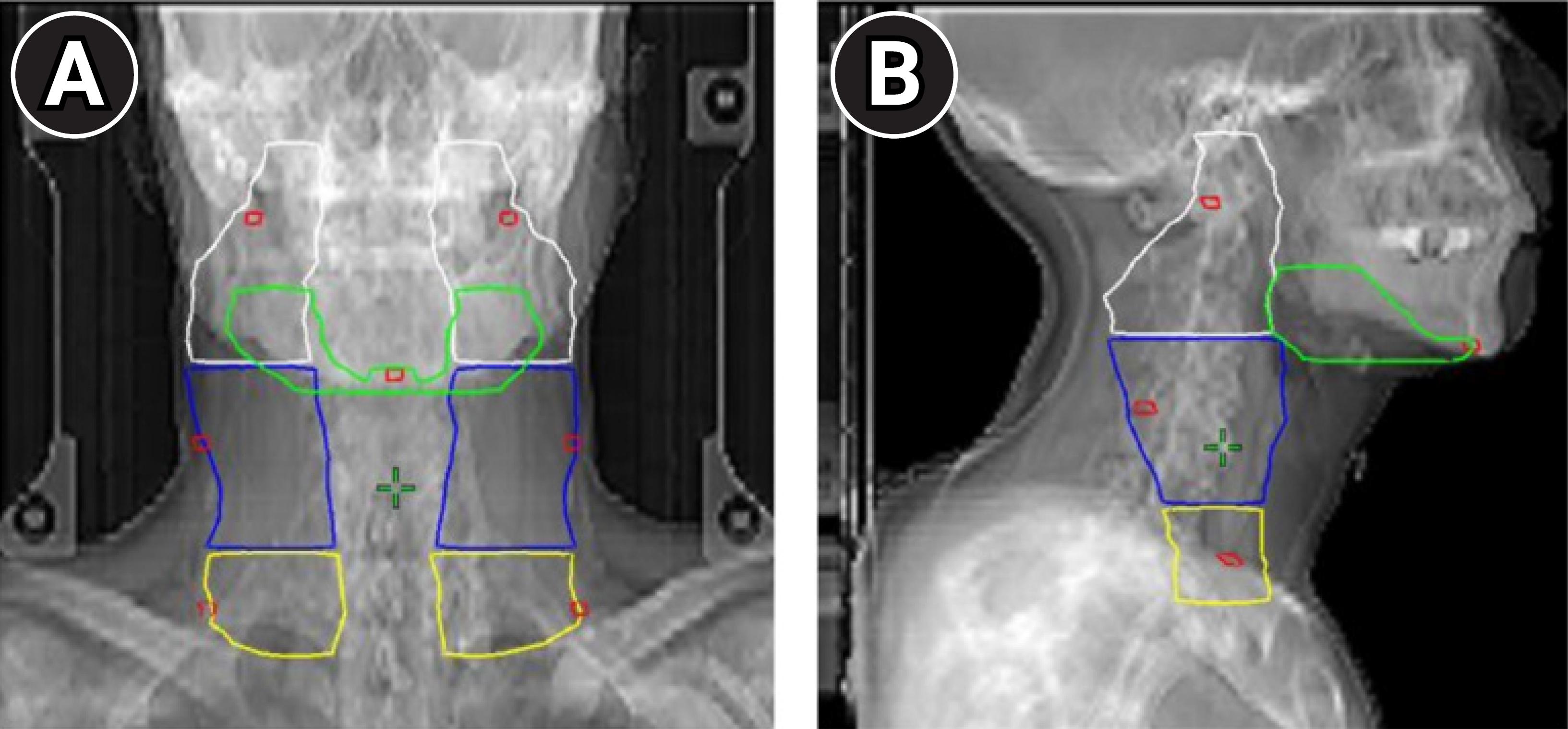
Fig.В 2.Population histogram for movement of the reference point corresponding to neck lymph node level I along three translational axes: (A) AP, (B) LR, (C) SI directions, and (D) overall RA magnitude. The red line indicates the point where the movement exceeds 3 mm. AP, anterior-posterior; LR, left-right; SI, superior-inferior; RA, radial, SD, standard deviation. 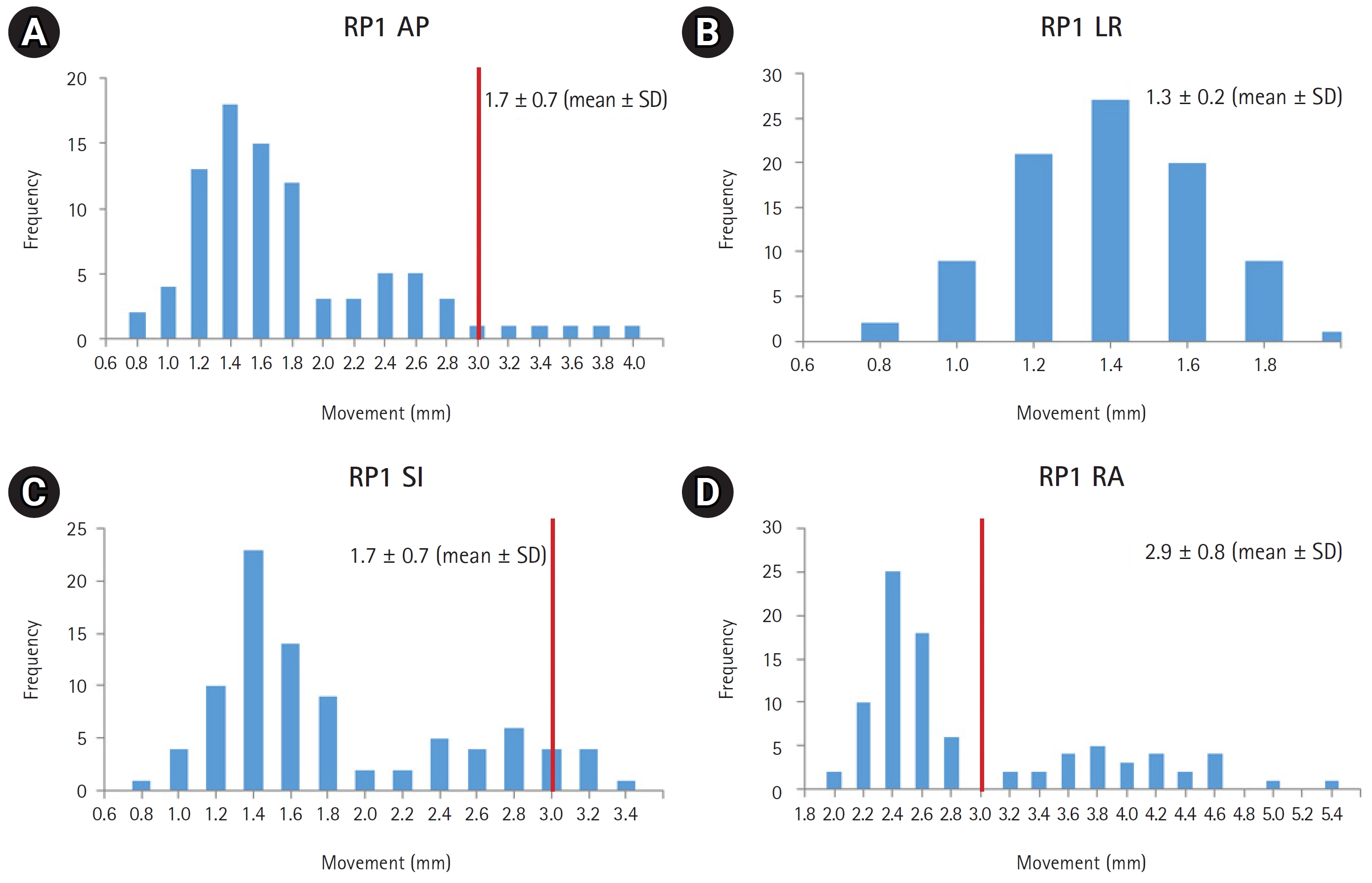
Fig.В 3.Population histogram for movement of the reference point corresponding to neck lymph node level II along three translational axes: (A) AP, (B) LR, (C) SI directions, and (D) overall RA magnitude. The red line indicates the point where the movement exceeds 3 mm. AP, anterior-posterior; LR, left-right; SI, superior-inferior; RA, radial, SD, standard deviation. 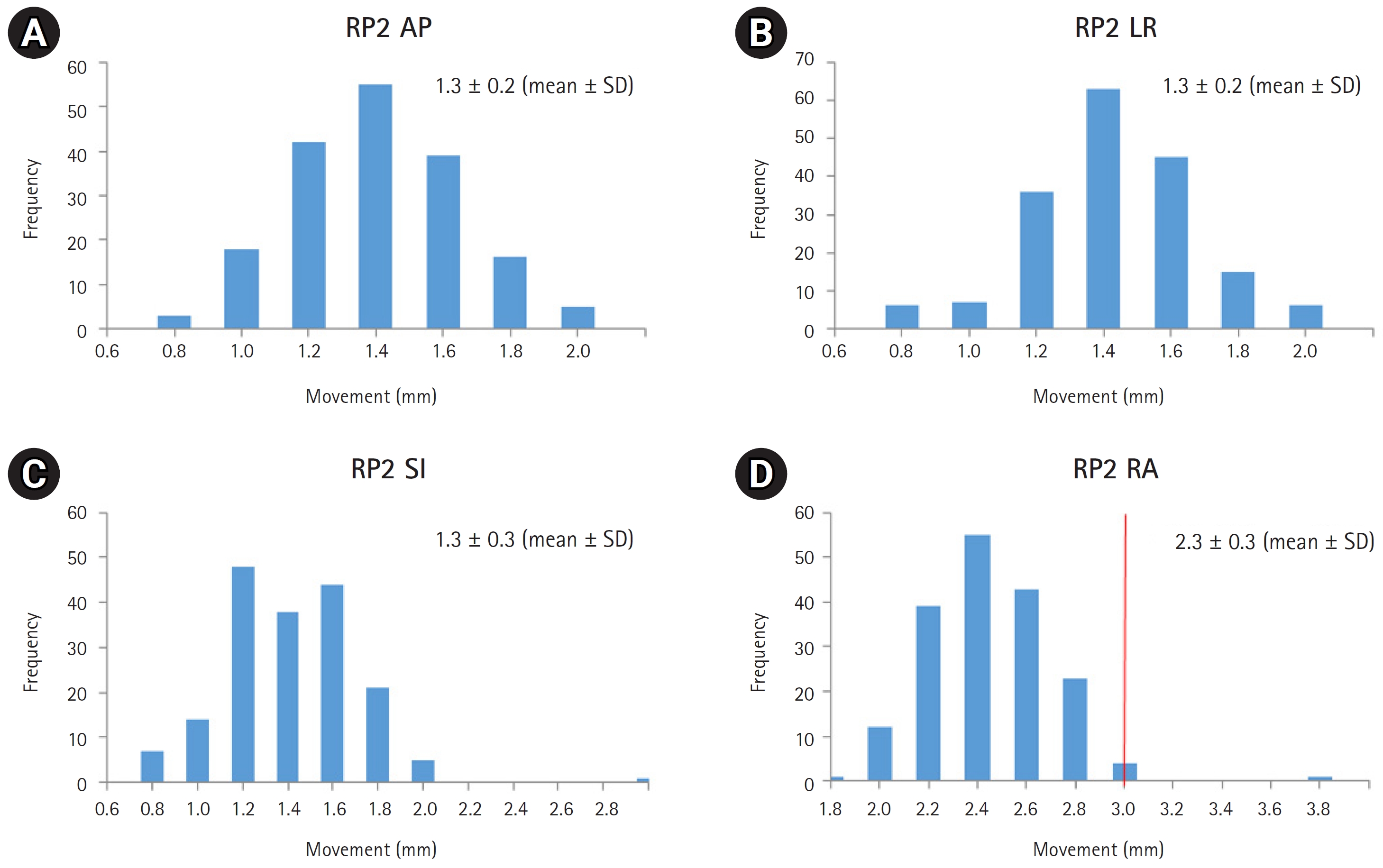
Fig.В 4.Population histogram for movement of the reference point corresponding to neck lymph node level III along three translational axes: (A) AP, (B) LR, (C) SI directions, and (D) overall RA magnitude. The red line indicates the point where the movement exceeds 3 mm. AP, anterior-posterior; LR, left-right; SI, superior-inferior; RA, radial, SD, standard deviation. 
Fig.В 5.Population histogram for movement of the reference point corresponding to neck lymph node level IV along three translational axes: (A) AP, (B) LR, (C) SI directions, and (D) overall RA magnitude. The red line indicates the point where the movement exceeds 3 mm. AP, anterior-posterior; LR, left-right; SI, superior-inferior; RA, radial, SD, standard deviation. 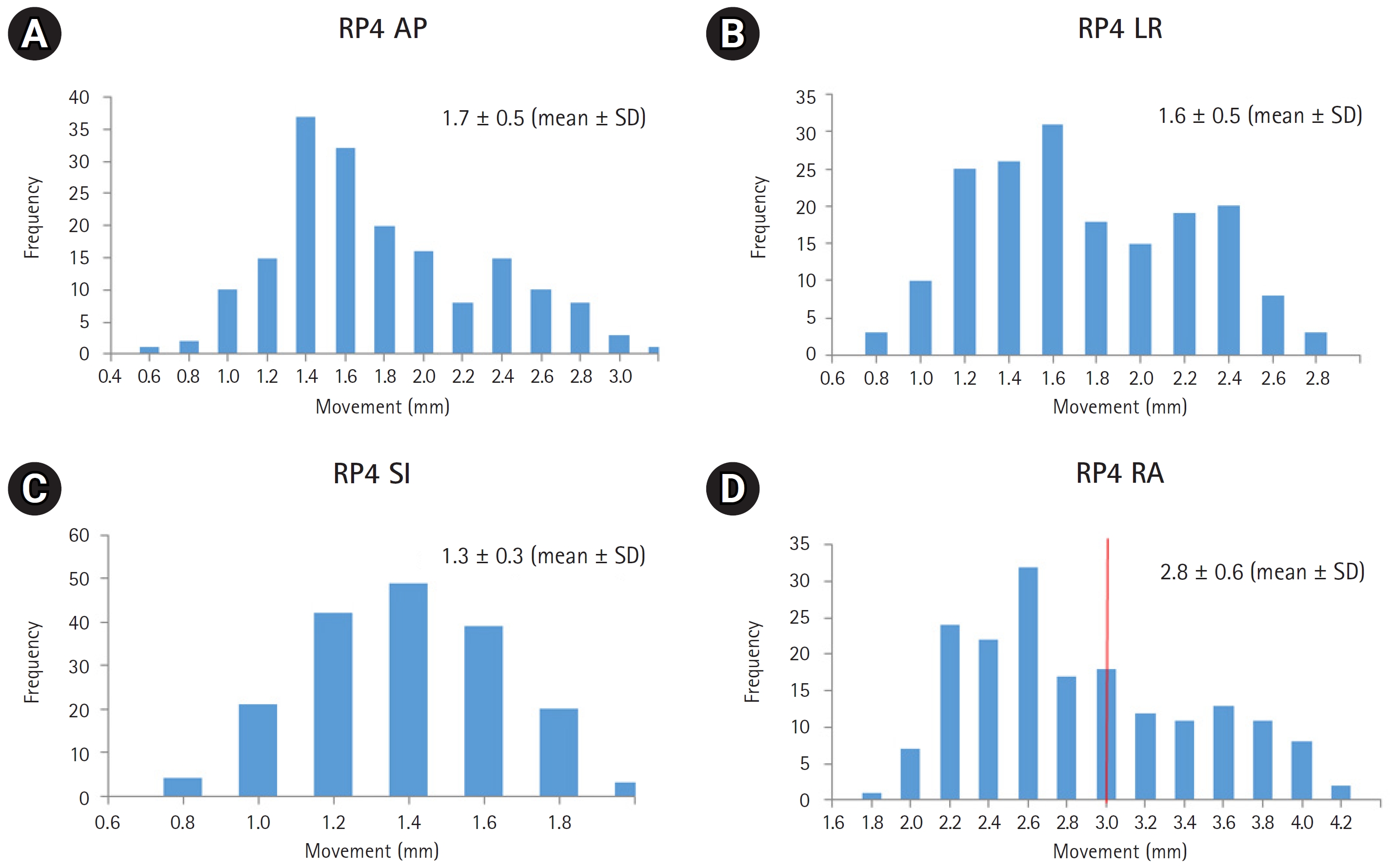
TableВ 1.Seven reference points of neck lymph node TableВ 2.Patient characteristics (n=89)
TableВ 3.Magnitude of deviation of each reference point (unit: mm) TableВ 4.Factors affecting the radial movement of each reference point by over 3 mm (unit: %) References1. Gormley M, Creaney G, Schache A, Ingarfield K, Conway DI. Reviewing the epidemiology of head and neck cancer: definitions, trends and risk factors. Br Dent J 2022;233:780вҖ“6.
3. Daly-Schveitzer N, Julieron M, Tao YG, Moussier A, Bourhis J. Intensity-modulated radiation therapy (IMRT): toward a new standard for radiation therapy of head and neck cancer? Eur Ann Otorhinolaryngol Head Neck Dis 2011;128:241вҖ“7.
4. Delishaj D, Ursino S, Pasqualetti F, et al. Set-up errors in head and neck cancer treated with IMRT technique assessed by cone-beam computed tomography: a feasible protocol. Radiat Oncol J 2018;36:54вҖ“62.
5. Gill SK, Reddy K, Campbell N, Chen C, Pearson D. Determination of optimal PTV margin for patients receiving CBCT-guided prostate IMRT: comparative analysis based on CBCT dose calculation with four different margins. J Appl Clin Med Phys 2015;16:252вҖ“62.
6. Gregoire V, Evans M, Le QT, et al. Delineation of the primary tumour Clinical Target Volumes (CTV-P) in laryngeal, hypopharyngeal, oropharyngeal and oral cavity squamous cell carcinoma: AIRO, CACA, DAHANCA, EORTC, GEORCC, GORTEC, HKNPCSG, HNCIG, IAG-KHT, LPRHHT, NCIC CTG, NCRI, NRG Oncology, PHNS, SBRT, SOMERA, SRO, SSHNO, TROG consensus guidelines. Radiother Oncol 2018;126:3вҖ“24.
7. Huang SH, OвҖҷSullivan B. Overview of the 8th edition TNM Classification for Head and Neck Cancer. Curr Treat Options Oncol 2017;18:40.
8. Koroulakis A, Jamal Z, Agarwal M. Anatomy, head and neck, lymph nodes. Treasure Island (FL): StatPearls Publishing; 2022.
9. Gupta T, Chopra S, Kadam A, et al. Assessment of three-dimensional set-up errors in conventional head and neck radiotherapy using electronic portal imaging device. Radiat Oncol 2007;2:44.
10. Strbac B, Jokic VS. Evaluation of set-up errors in head and neck radiotherapy using electronic portal imaging. Phys Med 2013;29:531вҖ“6.
11. Mesko S, Wang H, Tung S, et al. Estimating PTV margins in head and neck stereotactic ablative radiation therapy (SABR) through target site analysis of positioning and intrafractional accuracy. Int J Radiat Oncol Biol Phys 2020;106:185вҖ“93.
12. Huang YM, Lee JC, Chu CM, et al. Three-dimensional printed silicone bite blocks for radiotherapy of head and neck cancer: a preliminary study. Appl Sci 2020;10:1688.
13. Kil WJ, Kulasekere C, Derrwaldt R, Bugno J, Hatch C. Decreased radiation doses to tongue with вҖңstick-outвҖқ tongue position over neutral tongue position in head and neck cancer patients who refused or could not tolerate an intraoral device (bite-block, tongue blade, or mouthpiece) due to trismus, gag reflex, or discomfort during intensity-modulated radiation therapy. Oncotarget 2016;7:53029вҖ“36.
14. Anjanappa M, Rafi M, Bhasi S, et al. Setup uncertainties and PTV margins at different anatomical levels in intensity modulated radiotherapy for nasopharyngeal cancer. Rep Pract Oncol Radiother 2017;22:396вҖ“401.
15. Ishida R, Palmer JB, Hiiemae KM. Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia 2002;17:262вҖ“72.
16. Kendall KA, Leonard RJ. Hyoid movement during swallowing in older patients with dysphagia. Arch Otolaryngol Head Neck Surg 2001;127:1224вҖ“9.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||

 |
 |