 |
 |
AbstractPurposeOptimal radiotherapy treatment volumes for patients with locally advanced hypopharynx squamous cell carcinoma should ensure maximal tumor coverage with minimal inclusion of normal surrounding structures. Here we evaluated the effectiveness of a direct 3-mm high-dose gross tumor volume to planning target volume expansion on clinical outcomes for hypopharynx cancers.
Materials and MethodsWe performed a retrospective analysis of patients with hypopharynx carcinoma treated between 2004 and 2018 with primary radiotherapy using a direct high-dose gross tumor volume to planning target volume expansion and with or without concurrent systemic therapy. Diagnostic imaging of recurrences was co-registered with the planning CT. Spatial and volumetric analyses of contoured recurrences were compared with planned isodose lines. Failures were initially defined as in field, marginal, elective nodal, and out of field. Each failure was further classified as central high-dose, peripheral high-dose, central intermediate/low-dose, peripheral intermediate/low-dose, and extraneous. Clinical outcomes were analyzed by Kaplan-Meier estimation.
ResultsThirty-six patients were identified. At a median follow-up at 52.4 months, estimated 5-year overall survival was 59.3% (95% confidence interval [CI], 36.3%ŌĆō74.1%), 5-year local and nodal control was 71.7% (95% CI, 47.1%ŌĆō86.3%) and 69.9% (95% CI, 57.0%ŌĆō82.6%), respectively. The most common failure was in the high-dose primary target volume. The gastrostomy tube retention rate at 1 year among patients without recurrence was 13.0% (95% CI, 3.2%ŌĆō29.7%).
IntroductionIn the United States, there are approximately 3,000 patients per year diagnosed with hypopharynx cancer with most cases presenting with locally advanced disease [1,2]. Radiotherapy (RT)-based management of locally advanced disease is the predominant treatment approach [3]. The intimate association of the hypopharynx with dysphagia and aspiration risk structures (DARS) such as the larynx, pharyngeal constrictors, and cricopharyngeus muscle [4-8] challenges the normal tissue sparing capabilities associated with intensity-modulated radiotherapy (IMRT) [9]. This difficulty is further complicated by the submucosal extension and numerous pathways of tumor spread associated with hypopharynx cancers leading to recommendations for generous high- and intermediate-dose RT treatment volumes [10-12]. Therefore, patients with hypopharynx cancer treated with RT are at increased risk for developing significant long-term toxicities compared to other head and neck subsites [13,14].
There is limited data on patterns of failure in the IMRT era for patients receiving curative intent therapy for hypopharynx cancer. The series that have been reported, however, demonstrate favorable local control with most failures occurring within the high-dose clinical target volume (CTV) generated by a 5ŌĆō10 mm expansion from the gross tumor volume (GTV) [15,16]. Despite favorable local control, the large high-dose CTV increases dose to nearby DARS placing patients at risk for long-term aspiration and dysphagia. Alternative methods of reducing risk to DARS from high-dose RT beyond that achieved with IMRT-generated steep dose gradients are required.
We recently reported our experience of patients with oropharynx and larynx cancer treated with a high-dose planning target volume (PTV) created by a direct 3-mm expansion of the GTV without an intermittent high-dose CTV. The high-dose PTV was surrounded by an intermediate-dose CTV created by a 10-mm expansion of the GTV to cover microscopic tumor spread [17,18]. Local control was excellent in both oropharynx and larynx cohorts with nearly all failures occurring in the high-dose target volume and dose to adjacent organs-at-risk was decreased. Given the unique submucosal spread, tumor extension pathways, and anatomic relationship with DARS, the efficacy of minimal high-dose target volume expansion for patients with hypopharynx cancer was evaluated.
Materials and MethodsThis study was approved by the University of Wisconsin-Madison Institutional Review Board (No. UW17001). The informed consent was waived. We identified 36 patients with squamous cell carcinoma of the hypopharynx treated with definitive IMRT with or without systemic therapy between 2004 and 2018. The American Joint Committee on Cancer (AJCC) 8th staging system was used for reporting of patient data.
1. TreatmentPatients were immobilized with a thermoplastic head and neck mask for simulation using. Intravenous contrast was used unless medically contraindicated. The high-dose gross tumor volume (HD-GTV70Gy) included the primary tumor and pathologic lymph nodes determined by the treating radiation oncologist using physical exam findings and cross-sectional imaging. The intermediate-dose CTV (ID-CTV60Gy) was generated by a 10-mm expansion of the HD-GTV70Gy, trimmed from air, bone and areas considered as natural borders against tumor extension, and involved high-risk nodal stations. A low-dose CTV (LD-CTV54-56Gy) was used for prophylactic coverage of low-risk uninvolved nodal stations. HD-GTV70Gy and all CTVs were volumetrically expanded by 3 mm to create respective PTVs. Patients received radiotherapy to total doses of 70 Gy, 60ŌĆō63 Gy, and 54ŌĆō56 Gy to the HD-, ID-, and LD-PTVs, respectively, in 33ŌĆō35 fractions using TomoTherapy with daily CT image-guidance. The most common concurrent systemic therapies consisted of either weekly cisplatin at 30ŌĆō40 mg/m2, cisplatin at 100 mg/m2 given every three weeks, or cetuximab with a 400 mg/m2 loading dose followed by weekly doses of 250 mg/m2 weekly. Less common systemic regimens are listed in Table 1.
2. Patterns of failure determinationImaging at the time of failure was deformably co-registered with the treatment planning CT and 95% isodose lines using MIM software (MIM Software Inc., Cleveland, OH, USA) as previously described [19]. Failures were defined as in field, marginal, elective nodal, and out of field. Treatment volumes were further classified as central high-dose, peripheral high-dose, central intermediate/low-dose, peripheral intermediate/low-dose, and extraneous. If <95% of the contoured recurrent tumor volume was located within the 95% isodose line of the high-dose, intermediate-dose, or low-dose, it was considered a marginal failure. Conversely, if Ōēź to 95% of the volume was located within the 95% isodose line of the prescription, the failure was considered to be central.
3. StatisticsTime to local, regional, and distant failure was defined from the date of diagnosis. Overall survival, local and regional control, and gastrostomy tube placement was analyzed by the Kaplan-Meier method. Gastrostomy tube rate was analyzed for the subgroup of patients without recurrence or death at one year.
Results1. Patient data and clinical outcomesWe identified 36 patients with squamous cell carcinoma of the hypopharynx who received RT-based treatment. Patient, disease, and treatment characteristics are detailed in Table 1. At a median follow-up of 52.4 months, the estimated 5-year overall survival was 59.3% (95% confidence interval [CI], 36.3%ŌĆō74.1%). Five-year local and nodal control were 69.9% (95% CI, 57.0%ŌĆō82.6%) and 71.7% (95% CI, 47.1%ŌĆō86.3%), respectively (Fig. 1A, 1B).
2. Patterns of failureWe initially analyzed patterns of first recurrence in 15 patients who developed recurrent or metastatic disease. Seven patients developed metastatic disease of which two patients had isolated metastatic disease, four patients developed metastatic and nodal recurrence, and one patient developed primary and metastatic recurrence. There were eight locoregional recurrences with two in the primary and nodal regions and six with only primary recurrence. There were no isolated nodal recurrences in this cohort (Fig. 2A). Of the initial 15 recurrent patients, 13 had a component of locoregional failure with 12 having analyzable treatment plans. We further characterized these recurrences to determine if they occurred within the high-dose region defined as 95% of the recurrent tumor volume within the 95% isodose line of the 70 Gy field. We found that 9 of 12 analyzable failures occurred within the high-dose field with 8 of 9 occurring at the primary site. One failure was classified as marginal failure because only 91% of the failure was within the high-dose region. The recurrent lesion was well centered in the high-dose volume but did extend into the cervical esophagus inferiorly, which was out of the high-dose field (Fig. 3). One patient recurred in the intermediate dose elective region in level IV with additional widespread metastatic disease. The final recurrence was out of field in level V (Fig. 2B).
3. SalvageThirteen patients had a component of locoregional recurrence at first recurrence, eight were able to undergo salvage surgery. All salvage surgeries involved a total laryngectomy with five undergoing concurrent neck dissection. No patients developed isolated nodal failure; thus, no patients were salvaged with neck dissection alone. There was one perioperative death due to arrythmia with the rest of the salvage surgeries representing negative margin resections. The locoregional recurrence free survival at 1 year was 42.9% (95% CI, 9.8%ŌĆō73.5%). Ultimately six of seven patients who underwent savaged surgery experienced further locoregional recurrence. Overall survival at one year was 37.5% (95% CI, 8.8%ŌĆō67.5%) with a median overall survival of 9.3 months. One patient is alive without recurrence following salvage with 3.5 years of follow-up.
4. ToxicityLate toxicity data was gathered for 33 patients with at least 1 year of follow-up. The gastrostomy tube retention rate at 1 year among patients without recurrence was 13.0% (95% CI, 3.2%ŌĆō29.7%). Among patients without recurrence, only two patients required tracheostomy tube placement. One patient had a tracheostomy 6 months after radiation therapy due to laryngeal edema. A second patient had a tracheostomy prior to radiation therapy, which was removed after 3 months. Seven patients (21.2%) developed hypopharyngeal stricture requiring dilation. Seven patients also developed aspiration pneumonia (21.2%) while three additional patients developed aspiration without pneumonia.
Discussion and ConclusionRT-based management of hypopharynx cancer is well established and represents the most common treatment approach [3,20,21]. Historically, locoregional control rates of 40%ŌĆō70% were achieved with 2D and 3D conformal radiotherapy with or without systemic therapy [21-28]. These rates have been maintained or improved with decreased long-term toxicity using IMRT despite the risk for marginal misses given its inherent steep dose gradient. These series and current consensus guidelines [11] recommend a 0.5ŌĆō1.5 cm expansion of the GTV to create a high-dose CTV to account for subclinical tumor spread. We demonstrate that replacing a gross tumor and high-dose CTV with a GTV encompassed by a 1-cm intermediate-dose CTV resulted in clinical outcomes similar to other reported contemporaneous IMRT series that used larger high-dose target volumes. This approach was associated with excellent locoregional control and a favorable toxicity profile.
GTV expansions are created to account for tumor cells not apparent on imaging or direct visualization. Histopathologic data suggests that the extent of microscopic tumor spread beyond gross disease is 5 mm in greater than 90% of cases [29]. Primary tumor failures identified in this series were nearly all within the high-dose target volume suggesting that microscopic disease was sterilized by the intermediate dose expansion that received doses of approximately 60 Gy to 66 Gy, which are the recommended doses used for microscopic disease in the postoperative setting [30,31].
Beyond the sterilizing capacity of microscopic tumor extension using 60 Gy to 66 Gy in the definitive setting, another consideration for eliminating a high-dose GTV expansion is the documented discrepancy of histopathologic tumor volumes and those generated using modern imaging. In a robust study looking at resected hypopharynx specimens processed in a fashion to eliminate tissue retraction demonstrated that contoured GTVs on axial images generated by CT, MRI, and PET scans were all larger than the actual tumor [32]. Therefore, the contoured GTV receiving 70 Gy may in fact cover microscopic tumor extension.
In further support of limiting the 70 Gy volume to the GTV, recent data suggests that doses as low as 40 Gy (equivalent dose in 2 Gy fractions) is sufficient to sterilize microscopic tumor cells. In a randomized study of reduced dose to the elective neck in patients with head and neck squamous cell carcinomas, at 5 years there was no difference in overall survival, local control, regional control, nor distant metastases between those that received 40 Gy versus 50 Gy [33].
The proposed benefit of a refined high-dose target volume is reduced dose to DARS. Indeed, here we report 1-year gastrostomy tube retention of 13% and a 21% risk of aspiration induced pneumonia. These rates are similar to historical rates of 28% and 24% of gastrostomy tube dependence and aspiration induced pneumonia, respectively [34,35]. Additional patients are necessary to confirm a significant reduction in toxicity.
The interpretation of the results of this study must be interpreted in the context of its relatively small size and retrospective nature. We attempted to utilize objective metrics of toxicity to mitigate the uncertainty associated with interpreting toxicity from a retrospective study. These findings require confirmation in a prospective setting.
In conclusion, we demonstrate expected rates of locoregional disease control using minimal high-dose target volumes for patients with hypopharyngeal squamous cell carcinoma with favorable long-term toxicity. Despite these findings, patients with hypopharynx cancer exhibit worse clinical outcomes and toxicities compared to other head and neck disease sites. Therefore, there is a pressing need for novel approaches to improve clinical management and toxicity profiles.
AcknowledgmentsWe thank Heather M. Geye for maintaining the University of Wisconsin-Madison Head and Neck database.
NotesStatement of Ethics This study was approved by the University of Wisconsin-Madison Institutional Review Board (No. UW17001). Financial Support This work was supported in part by the Wisconsin Head & Neck Cancer SPORE (No. P50DE026787). Author Contribution Conceptualization, MW, AB. Funding acquisition, PH, RK. Investigation and methodology, MW, AB. Writing of the original draft, AB. Writing of the review and editing, MW, PH, RK, AW, GH. Formal analysis, AB, PH, MW. Data curation, AB. All the authors have proofread the final version. Fig.┬Ā1.Clinical outcomes of hypopharynx patients treated with a minimal high-dose radiation target volume. (A) Overall survival at 5 years was 59.3% (95% CI, 36.3%ŌĆō74.1%). (B) Local and nodal control at 5 years was 69.9% (95% CI, 57.0%ŌĆō82.6%) and 71.7% (95% CI, 47.1%ŌĆō86.3%), respectively. CI, confidence interval. 
Fig.┬Ā2.(A) Venn diagram depicting location of first failure. (B) Diagram depicting types of failure. In field is defined when 95% of the recurrence occurred within the 95% isodose line of the highest dose region. Marginal failure is defined when the recurrence was is in the high-dose region but <95% of the recurrence was contained within the 95% isodose line of the highest dose region. Elective failure is defined when the recurrence occurs in a low-dose region. Out of field failure is defined by a recurrence in a nodal region not receiving radiation. 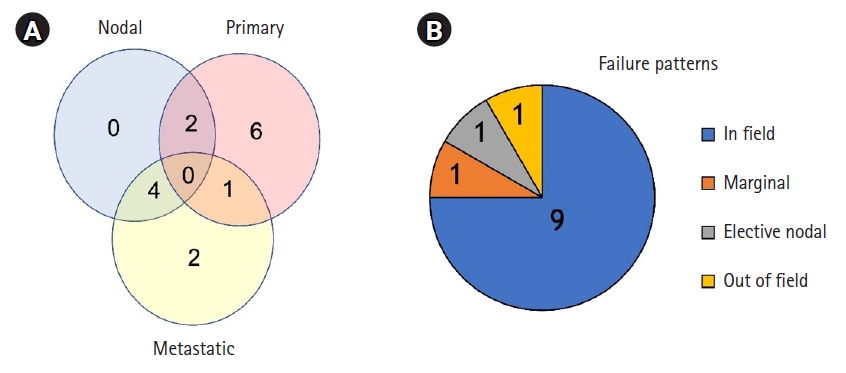
Fig.┬Ā3.A single marginal failure was identified. Green represents the planning target volume, and the red outline corresponds to the contoured recurrence. It was classified as a marginal failure because only 91% of the failure was within the high-dose region. 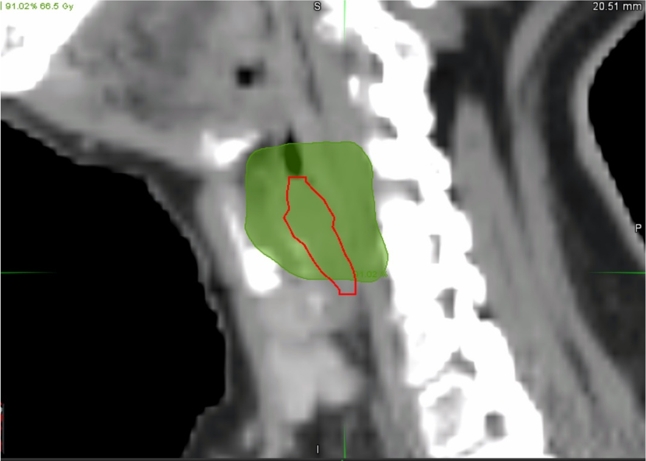
Table┬Ā1.Patient and treatment characteristics References1. American Cancer Society. Cancer Facts & Figures [Internet]. Atlanta, GA: American Cancer Society; 2021 [cited 2022 Sep 23]. Available from: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2021.html.
2. Hoffman HT, Karnell LH, Shah JP, et al. Hypopharyngeal cancer patient care evaluation. Laryngoscope 1997;107:1005ŌĆō17.
3. The American College of Surgeons benchmark report: the National Cancer Database [Internet]. Chicago, IL: American College of Surgeons; 2011, pp[cited 2022 Sep 23]. Available from: https://www.facs.org/quality-programs/cancer-programs/national-cancer-database/.
4. Caglar HB, Tishler RB, Othus M, et al. Dose to larynx predicts for swallowing complications after intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 2008;72:1110ŌĆō8.
5. Eisbruch A, Schwartz M, Rasch C, et al. Dysphagia and aspiration after chemoradiotherapy for head-and-neck cancer: which anatomic structures are affected and can they be spared by IMRT? Int J Radiat Oncol Biol Phys 2004;60:1425ŌĆō39.
6. Jensen K, Lambertsen K, Grau C. Late swallowing dysfunction and dysphagia after radiotherapy for pharynx cancer: frequency, intensity and correlation with dose and volume parameters. Radiother Oncol 2007;85:74ŌĆō82.
7. OŌĆÖHare J, Maclean J, Szczesniak M, et al. Laryngeal tumours and radiotherapy dose to the cricopharyngeus are predictive of death from aspiration pneumonia. Oral Oncol 2017;64:9ŌĆō14.
8. Rancati T, Schwarz M, Allen AM, et al. Radiation dose-volume effects in the larynx and pharynx. Int J Radiat Oncol Biol Phys 2010;76(3 Suppl):S64ŌĆō9.
9. Lee N, Puri DR, Blanco AI, Chao KS. Intensity-modulated radiation therapy in head and neck cancers: an update. Head Neck 2007;29:387ŌĆō400.
10. Eisbruch A, Foote RL, OŌĆÖSullivan B, Beitler JJ, Vikram B. Intensity-modulated radiation therapy for head and neck cancer: emphasis on the selection and delineation of the targets. Semin Radiat Oncol 2002;12:238ŌĆō49.
11. Gregoire V, Evans M, Le QT, et al. Delineation of the primary tumour Clinical Target Volumes (CTV-P) in laryngeal, hypopharyngeal, oropharyngeal and oral cavity squamous cell carcinoma: AIRO, CACA, DAHANCA, EORTC, GEORCC, GORTEC, HKNPCSG, HNCIG, IAG-KHT, LPRHHT, NCIC CTG, NCRI, NRG Oncology, PHNS, SBRT, SOMERA, SRO, SSHNO, TROG consensus guidelines. Radiother Oncol 2018;126:3ŌĆō24.
12. Lapeyre M, Bailly C, Toledano I, Montalban A, Russier M. Hypopharynx and larynx cancers: propositions for the selection and the delineation of peritumoral microscopic disease volumes (lymph nodes excluded). Cancer Radiother 2010;14 Suppl 1:S43ŌĆō51.
13. Langerman A, Maccracken E, Kasza K, Haraf DJ, Vokes EE, Stenson KM. Aspiration in chemoradiated patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 2007;133:1289ŌĆō95.
14. Machtay M, Moughan J, Farach A, et al. Hypopharyngeal dose is associated with severe late toxicity in locally advanced head-and-neck cancer: an RTOG analysis. Int J Radiat Oncol Biol Phys 2012;84:983ŌĆō9.
15. Daly ME, Le QT, Jain AK, et al. Intensity-modulated radiotherapy for locally advanced cancers of the larynx and hypopharynx. Head Neck 2011;33:103ŌĆō11.
16. Studer G, Lutolf UM, Davis JB, Glanzmann C. IMRT in hypopharyngeal tumors. Strahlenther Onkol 2006;182:331ŌĆō5.
17. Burr AR, Harari PM, Haasl AM, et al. Clinical outcomes for larynx patients with cancer treated with refinement of high-dose radiation treatment volumes. Head Neck 2020;42:1874ŌĆō81.
18. Burr AR, Harari PM, Ko HC, Bruce JY, Kimple RJ, Witek ME. Reducing radiotherapy target volume expansion for patients with HPV-associated oropharyngeal cancer. Oral Oncol 2019;92:52ŌĆō6.
19. Mohamed AS, Rosenthal DI, Awan MJ, et al. Methodology for analysis and reporting patterns of failure in the Era of IMRT: head and neck cancer applications. Radiat Oncol 2016;11:95.
20. Lefebvre JL, Andry G, Chevalier D, et al. Laryngeal preservation with induction chemotherapy for hypopharyngeal squamous cell carcinoma: 10-year results of EORTC trial 24891. Ann Oncol 2012;23:2708ŌĆō14.
21. Lefebvre JL, Chevalier D, Luboinski B, Kirkpatrick A, Collette L, Sahmoud T. Larynx preservation in pyriform sinus cancer: preliminary results of a European Organization for Research and Treatment of Cancer phase III trial. EORTC Head and Neck Cancer Cooperative Group. J Natl Cancer Inst 1996;88:890ŌĆō9.
22. Bahadur S, Thakar A, Mohanti BK, Lal P. Results of radiotherapy with, or without, salvage surgery versus combined surgery and radiotherapy in advanced carcinoma of the hypopharynx. J Laryngol Otol 2002;116:29ŌĆō32.
23. Featherstone CJ, Clarke S, Jackson MA, et al. Treatment of advanced cancer of the larynx and hypopharynx with chemoradiation. ANZ J Surg 2004;74:554ŌĆō8.
24. Hall SF, Groome PA, Irish J, OŌĆÖSullivan B. The natural history of patients with squamous cell carcinoma of the hypopharynx. Laryngoscope 2008;118:1362ŌĆō71.
25. Kim S, Wu HG, Heo DS, Kim KH, Sung MW, Park CI. Advanced hypopharyngeal carcinoma treatment results according to treatment modalities. Head Neck 2001;23:713ŌĆō7.
26. Lefebvre JL, Pointreau Y, Rolland F, et al. Induction chemotherapy followed by either chemoradiotherapy or bioradiotherapy for larynx preservation: the TREMPLIN randomized phase II study. J Clin Oncol 2013;31:853ŌĆō9.
27. Samant S, Kumar P, Wan J, et al. Concomitant radiation therapy and targeted cisplatin chemotherapy for the treatment of advanced pyriform sinus carcinoma: disease control and preservation of organ function. Head Neck 1999;21:595ŌĆō601.
28. Zelefsky MJ, Kraus DH, Pfister DG, et al. Combined chemotherapy and radiotherapy versus surgery and postoperative radiotherapy for advanced hypopharyngeal cancer. Head Neck 1996;18:405ŌĆō11.
29. Fleury B, Thariat J, Barnoud R, et al. Microscopic extensions of head and neck squamous cell carcinomas: impact for clinical target volume definition. Cancer Radiother 2014;18:666ŌĆō71.
30. Bernier J, Domenge C, Ozsahin M, et al. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med 2004;350:1945ŌĆō52.
31. Cooper JS, Zhang Q, Pajak TF, et al. Long-term follow-up of the RTOG 9501/intergroup phase III trial: postoperative concurrent radiation therapy and chemotherapy in high-risk squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 2012;84:1198ŌĆō205.
32. Daisne JF, Duprez T, Weynand B, et al. Tumor volume in pharyngolaryngeal squamous cell carcinoma: comparison at CT, MR imaging, and FDG PET and validation with surgical specimen. Radiology 2004;233:93ŌĆō100.
33. Deschuymer S, Nevens D, Duprez F, et al. Randomized clinical trial on reduction of radiotherapy dose to the elective neck in head and neck squamous cell carcinoma; update of the long-term tumor outcome. Radiother Oncol 2020;143:24ŌĆō9.
|
|
|||||||||||||||||||||||||||||||||||||||||

 |
 |